Implementation
Successful implementation of advance care planning requires culture change and a whole-of-system approach.
The following steps and resources will assist you to implement advance care planning and shared goals of care in your area.
Our interactive advance care planning services map contains an email contact in your local district (DHB) to support your advance care planning implementation efforts, as well as an indication of the DHB process for uploading advance care plans.
Having clinical staff who are skilled and confident to support people with advance care planning is essential.
Training alone will not create sustainable change in practice. We need trained clinicians to have the conversations and use the information gathered to inform care.
This requires the development of a system within your Te Whatu Ora district or clinical area that includes all of these key elements:
• leadership to champion for the programme and source people and resources that might be required
• a process for identifying people who would benefit
• clinicians supported to engage in the conversations with time, training and mentoring
• patients and their whānau supported before, during and after these conversations
• conversations documented effectively to inform care/treatment that aligns with what is important to the person and their whānau
• process to share and review plans with the person and with other health care providers
• process to ensure what is important to the person and their whānau is used in care planning and delivery
• process to review and continuously improve your advance care planning and shared goals of care practices.
Te Whatu Ora Implementation Guide
This implementation guide is designed to help Te Whatu Ora districts deliver advance care planning to the people they serve. It is a practical, ‘hands-on’ tool for Te Whatu Ora to use to generate ideas and find inspiration as they implement advance care planning
Created in response to feedback
The guide was created in response to feedback received during the development of the National ACP Strategy 2018–22. Click here to download the current 5 year strategy.
The National ACP Cooperative consistently heard that district health board (now Te Whatu Ora) deployment teams wanted:
a better understanding of how to provide advance care planning services (‘the deployment model’)
to be able to learn from each other
to share what they have done: what worked and how they overcame the challenges they encountered.
The development of a ‘how-to’ guide was therefore included in the strategy’s roadmap of action.
A work in progress
The guide is a ‘living’ resource and is not exhaustive. The ideas and activities it contains are recommendations only and designed to complement the district examples.
We will continuously build on the guide, adding more ideas and examples as teams, districts and communities try new approaches and overcome challenges and barriers through the various stages of ACP implementation.
Feedback
We welcome all feedback on the guide – please email acp@hqsc.govt.nz.
* In the guide, when we refer to DHBs, we mean the health system of a district not just the publicly funded providers within a district.
Overview of the guide
-
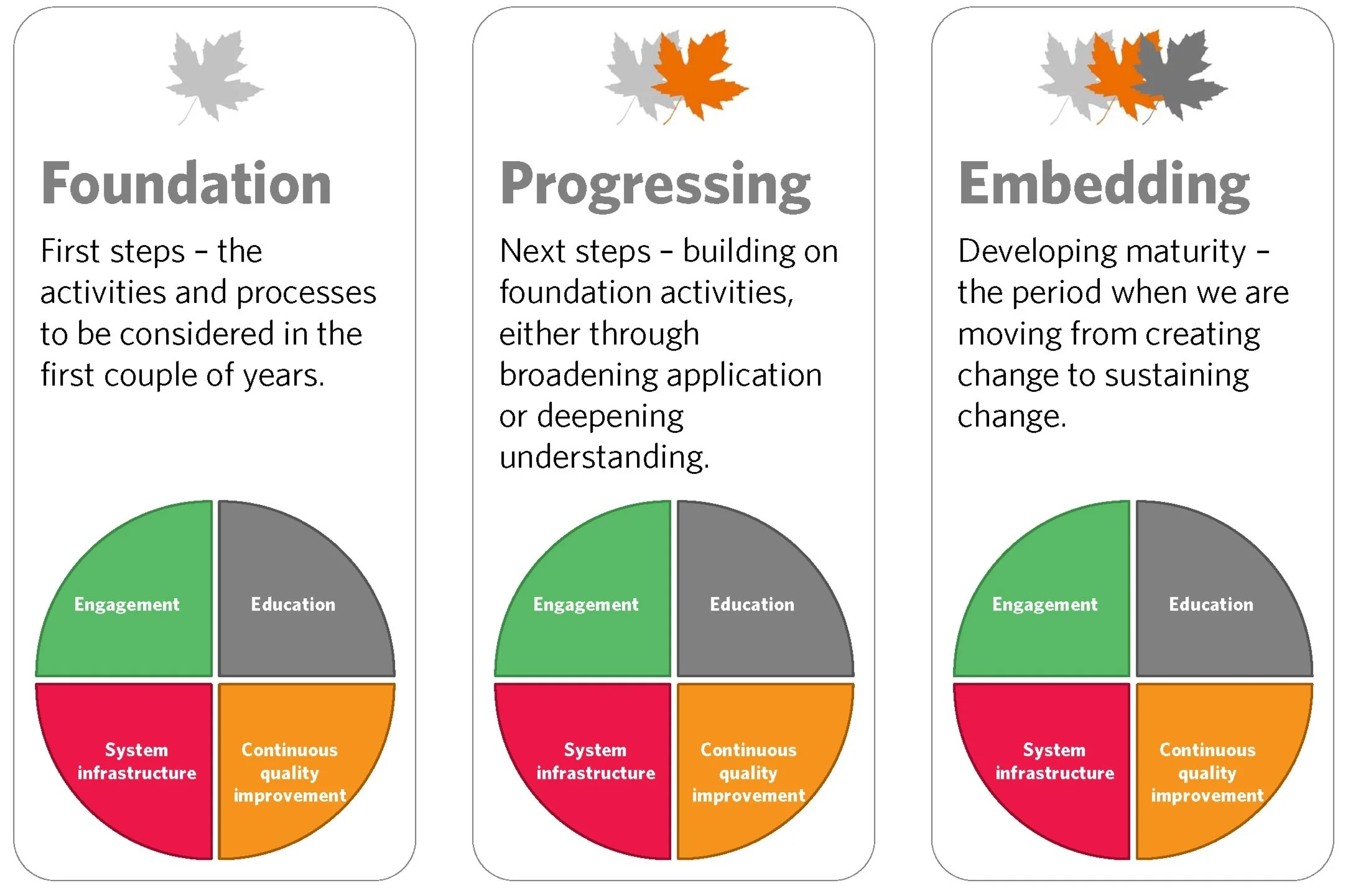
We have structured the guide around the three stages of ‘implementation maturity’ organisations may be at (foundation, progressing, embedding) in activities and processes associated with each of the four quadrants that make up the ‘deployment model’ (engagement, education, system infrastructure and continuous quality improvement).
The guide includes links to downloadable and printable examples of different approaches to ACP implementation taken by DHBs. They follow a set format:
• Why/rational
• By who
• Value added
• Risks/challenges they encountered along the way
• The steps they took
• Impact/outcomes
• Future opportunities. -
We have organised the guide content so you can ‘mix and match’ examples to suit the implementation stage you are at in the quadrants and the decisions you wish to make. Most of you will be at different stages within and between the various quadrants. For example, you may be at foundation stage in system infrastructure, but at progressing stage with engagement and education.
We recommend you start with the implementation process overview, regardless of which stage you are at. This gives you an introduction to each implementation stage and the four deployment quadrants, and measures of success in each.
We recommend you then explore each of the foundation, progressing and embedding pages. Each page includes examples of actions that you can take in relation to different parts of the sector, according to each of the four quadrants. There are also links to relevant downloadable resources.
Each resource describes an activity undertaken by a Whatu Ora.
Overview of the process
Adapted from Health Canada, March 2008
-
Effective ACP implementation requires a whole-of-system response that is coordinated, integrated and underpinned by quality assurance. The response will consistently and effectively support New Zealand consumers across the health system to think about, talk about and plan for their future and end-of-life care.
To support such a response, the ACP programme has drawn on national and international experience and developed a deployment model. This is a high-level guide to the things that need to be considered for ACP to be successfully implemented in New Zealand.
The system-wide change ACP requires over many years can appear overwhelming for steering groups, deployment teams and managers. So, to help break down the deployment model into more manageable chunks, we have created three stages or levels of implementation maturity – foundation, progressing and embedding – and applied them to the activities and processed associated with each of the four quadrants.
-
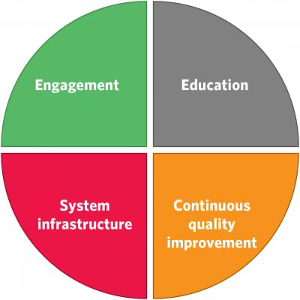
The deployment model acknowledges that we need appropriate policies and resources to underpin deployment. It focuses on four key areas or quadrants – engagement, education, system infrastructure and continuous quality improvement.
Successful change requires a structured and managed approach. The deployment model is built on the idea that, to deliver a whole-of-system change like ACP and make it ‘business as usual’, providers need to think about and address a number of different areas simultaneously. They need to:
• engage people in the need to change
• overcome any obstacles to the change
• build processes to support and sustain the change.This approach is consistent with systems thinking and large-scale change literature. It also maps to Kotter’s 8-Step Process for Leading Change.
-
1) Engagement
The engagement quadrant focuses on promoting ACP to the general public and health care sector. It aims to normalise future care planning.
At an organisational level, engagement requires the getting and retaining of support and involvement of health care leadership. At a community level, it requires engaging the general public in ACP development, deployment and participation.
Measuring success –We will know we are improving in this area when:
Consumers are:
• bringing up the topic of ACP or seeking clarification about future care options from health care providers and relevant others
• expecting to have ACP conversations as part of whole-person care
• expecting what matters to them to form the basis of care and partnership in decision-making (includes compassionate communication, information delivered in culturally appropriate ways and power sharing)Organisational leaders are:
• advocating for and prioritising ACP (creating an expectation/mandate)
• empowering consumers with information, tools and an empathetic care team (skilled to communicate and support consumers).
2) EducationThe education quadrant focuses on increasing the skills and knowledge of the health workforce and consumers.
Our health workforce requires training in ACP and support so they can initiate, participate in and facilitate ACP with consumers. This includes a working knowledge of the legal framework, good clinical communication skills and an understanding of associated systems and processes.
Consumers need information, training and resources to understand ACP, what the benefits are in planning their future care and what they need to be thinking about and planning for.
Communities, whānau and carers need skills and resources to effectively and appropriately support people to think about and talk about what matters most to them and how that might impact their preferences in the future.
Measuring success – We will know we are improving in this area when:
Consumers are:
• developing advance care plans regardless of geographic location, ethnicity or socioeconomic situation
• co-leading ACP programmes (with knowledge and confidence) within organisations (includes projects, steering groups, co-design, generating ideas, sharing stories and initiating ACP activities)
• confidently supporting others in their family/whānau and community to start ACPHealth and social care workers:
• are aware of their role in ACP and advocating for the consumer voice and in shared decision-making
• feel capable and confident, and are competent in their role in ACP (clinical decision-making, ACP knowledge and communication skills)
• know where to find advance care plans and how to use ACP to underpin care delivery
• role-modelling shared decision-making and values-based care planning.
3) System infrastructureThe system infrastructure quadrant focuses on the systems and processes required to maximise the investment in ACP and training so what is important to consumers is recorded, shared and valued.
Measuring success –We will know we are improving in this area when:
• treating clinicians and other health care workers are aware of and use consumer preferences and advance directives
• a central repository is developed to store ACP conversations and completed plans together with an alert or notification that they are there
• there is a linked-up system of ACP records and accessibility reflected in local processes and policies for documentation, retrieval and reviewing ACP conversations and plans. Local systems are consistent and link with national processes and policies
• completed advance care plans are quality assured.
4) Continuous quality improvement
The continuous quality improvement quadrant focuses on developing an ACP culture that uses measurement and evaluation tools to determine quality processes and applies them practically for quality improvement. The processes must be based on what matters to consumers.Measuring success – We will know we are improving in this area when:
• DHBs have ACP policies and protocols in place, and adherence is monitored
• sufficient human resources are allocated to drive the system changes required in DHBs
• process and outcome measures are tracked and opportunities for improvement are acted on. -
1) Foundation
First steps. These are the activities and processes to be considered in the first couple of years. They include building a guiding team, creating a platform and desire for change, going where people are willing, trying/piloting and sharing the small wins to build momentum.
View foundation activities and downloadable resources here
2) Progressing
The next steps building on foundation activities, either through broadening application or deepening understanding. Activities include increasing the quantity and quality of ACP, building on wins, sharing successes, widening advocacy and building clinical leadership.
View progressing activities and downloadable resources here
3) Embedding
Developing maturity. This is the period when we are moving from creating change to sustaining change. ACP becomes business as usual, an expected activity, and there is entrenched clinical leadership.
View embedding activities and downloadable resources here
Mixed stages
Note that teams, departments and DHBs may be at different stages within and between the various quadrants. Some examples follow.
Within quadrant:
• You might have great clinical leadership (embedding within the engagement quadrant) but only be starting community presentations (foundation in the engagement quadrant).
• You may have a robust electronic ACP process and systems in the hospital (embedding in the systems quadrant) but have no system or process for making those electronic advance care plans available to community health teams (foundation in the systems quadrant).Between quadrants:
• You may have trained many of your clinicians and have a waiting list for clinicians wanting to do training (embedding in the education quadrant) but no mandate or expectation that clinicians initiate ACP conversations (foundation in the engagement quadrant).
• You might have GPs who are actively creating advance care plans with consumers (embedding in the engagement and systems quadrants) but have no way of measuring that or checking the quality of those plans (foundation in the continuous quality improvement quadrant).
Foundation
Below are the activities and processes to be considered in the first couple of years of implementation, such as building a guiding team, creating a platform and desire for change, going where people are willing, trying/piloting and sharing the small wins to build momentum.
The ‘foundation’ actions listed below for different parts of the sector relate to each of the four quadrants. Links to downloadable associated resources and case studies are included.
Note that teams, departments and Te Whatu Ora may be at different stages within and between the various quadrants.
-
Focuses on promoting ACP to the general public and health care sector; normalising future care planning.
Community actions:
• Approach local community groups, eg, service groups, church groups, etc, and offer an ACP presentation.
• Offer consumers opportunities to attend local ACP presentations at community venues, local groups, aged residential care facilities, etc.
Health workforce management actions:
• Support management to value ACP and release staff to attend ACP training and participate in ACP initiatives/processes.
• Present at Grand Round/DHB board meetings etc, to garner support.
Health workforce actions:
• Develop an activity plan for participation in Advance Care Planning Day. Help to organise local activities, ideas and share print resources, such as posters, postcards, etc.
Downloadable resources and case studies:
• A cup of tea with ACP
• Raising ACP awareness in the legal sector
• Quarterly ACP reporting to the region
• Consumer ACP presentations
• Referral process for specialist ACP support• Still to come:
– 1 Engaging leadership
– 2 National initiatives that support ACP
– 17 ARRC engagement -
Focuses on increasing the skills and knowledge of the health workforce and consumers.
Community actions:
• Create generic consumer presentations tailored to recognise the diverse needs of the community.
• Promote the use of online ACP information and resources.
• Work alongside the national ACP team to develop community capacity for the national community training model.
– Recruit a team of volunteers for training.Health workforce management actions:
• Work alongside the national ACP team to develop local capacity for the national training model.
• Recruit skilled staff for facilitation training by developing processes for:
– advertising the training
– recruiting appropriate participants for training
– reviewing applications for training
– supporting trained staff.• Create a generic presentation for the health workforce outlining local processes (such as where to find a plan, how to recognise when to use the plan to support care, etc), which can be adapted to meet the needs of different parts of the workforce (eg, specialty, professions, etc).
• Promote use of online ACP information and resources (eg, advance care plan and guide, brochures, level 1 modules, etc).
Downloadable resources and case studies:
• ACP education for nursing staff
• Educating SMO on ACP legal aspects
• ACP in undergraduate medical training (Minnesota example)
• Still to come:
– 14 L2 training development
– 21 Increasing ACP in the outpatient clinic environment -
Focuses on the systems and processes required to maximise the investment in ACP and training so what is important to consumers is recorded, shared and valued.
Actions:
• Consider how advance care plans and ACP conversations will be identified in your DHB.
• Clarify who needs to have access to an advance care plan and how this might be supported.
– Consider are there new or existing networks or IT systems that can be tapped into or used?
– Or will you create paper-based processes?• Consider having a dedicated ACP budget for training, presentations and printing.
• Identify key/priority areas to target ACP local and national training initiatives.
• Appoint a DHB ACP coordinator (this may not be a full-time role in smaller DHBs).
• Identify where the national ACP resources (guide, brochures, etc) are received in your area, where they are kept and how they are distributed.
• Evaluate how local processes will link with national policies and processes.
• Identify who the target audience is for ACP in your DHB. There may be a different focus at different times (eg, chronic conditions, palliative care, the ‘surprise question’, etc).
• Establish a local steering group and appoint a clinical lead.
Downloadable resources and case studies:
• Including ACP in the electronic discharge summary
• ACP hospital alert and recording system
• ACP subsidy for general practice
• Formation of ACP Advisory Group
• Establishing an ACP mentoring system
• ACP funding for general practice
• Regional and district ACP integration
• ACP resource distribution through existing channels
• Map of Medicine - developing regional ACP pathway
• Nurse-led clinics in general practice
• Electronic System to share ACP
• Still to come:
o 11 ACP implementation guide in ARRC
o 30 ACP progress note -
Focuses on developing an ACP culture that uses measurement and evaluation tools to determine quality processes and applies them practically for quality improvement.
Actions:
• Define your DHB’s parameters regarding quality. Does it have a baseline for quality of advance care plans and processes?
• Define measures:
– What data is your DHB going to collect?
– How will you collect it?
– Who are you sharing this data with? Eg, DHB annual plan, regional service plan, quality accounts, etc.
– What format will it be shared in? Eg, raw data, graphs, etc.
–How will these link with national measures?• Develop a baseline of ACP preparedness.
• If issues are identified with advance care plans or processes within your DHB:
– who should be made aware?
– who is responsible for following up?
– who will be advised when the issue is resolved and/or further follow-up is identified as being needed?Downloadable resources and case studies:
• A ward-based ACP intervention
• ACP clinical review of plans
• Developing a baseline ACP survey
Progressing
These are the next steps building on foundation activities, either through broadening application or deepening understanding. Activities include increasing the quantity and quality of advance care planning, building on wins, sharing successes, widening advocacy and building clinical leadership.
The actions below relate to ‘progressing’ activities in each of the four quadrants for different parts of the sector. Links to downloadable associated resources and case studies are included.
Note that teams, departments and Te Whatu Ora may be at different stages within and between the various quadrants.
-
Focuses on promoting ACP to the general public and health care sector; normalising future care planning.
Community actions:
• Consumers are supported and encouraged to raise ACP with health care providers and relevant others.
• Presentations are given to relevant consumer groups (eg, service groups, church groups, community groups, etc).
Social sector actions:
• Develop opportunities for collaboration across health, social and other sectors.
Health workforce management actions:
• Create an expectation that what matters to consumers informs health care planning.
• Promote the benefits of ACP and future health care planning within DHBs to providers, non-governmental organisations, aged residential care facilities, primary health organisations, general practice and community groups.
• Socialise ACP at orientation and inductions across the health workforce.
Health workforce actions:
• Collect ACP stories and share successes.
• Workforce staff are approached and supported to organise and participate in ACP promotions.
• Plan for regular ACP articles and patient stories to feature in publications (eg, chief executive updates, quality accounts, local publications, etc).
Downloadable resources and case studies:
• Referral process for specialist ACP support
• Implementing electronic ACPs - Case study
• Still to come:
– 17 ARRC engagement
– 36 Waka model -
Focuses on increasing the skills and knowledge of the health workforce and consumers.
Community actions:
• Support volunteers to work with the community and consumers.
Health workforce actions:
• Establish infrastructure, processes and policies to support locally trained ACP facilitators to deliver ACP in your DHB and maximise the value of the training, ie, tracking conversations.
• Engage and educate the health workforce and give them the tools to initiate, participate and facilitate ACP.
• Incorporate level 1 e-learning modules into continuous education processes.
• Existing level 2 practitioners mentor and support other staff with ACP activities and conversations.
Downloadable resources and case studies:
• ACP education for nursing staff
• ACP in undergraduate medical training (Minnesota example)
• Implementing electronic ACPs - Case study
• Still to come:
– 20 ARC education
– 21 Increasing ACP in the outpatient clinic environment
– 36 Waka model -
Focuses on the systems and processes required to maximise the investment in ACP and training so what is important to consumers is recorded, shared and valued.
Actions:
• Incorporate ACP into established systems and processes (eg, annual performance appraisals for health workforce staff).
• Develop and implement processes to support the strategic advertisement and selection of staff to attend ACP training at both a local and national level.
• Develop a regional ACP network linking with representatives from each DHB in your region to:
– network
– share ideas and activities
– distribute ACP communications, information and updates.• Cultivate conversations with IT providers/DHB IT leadership regarding electronic ACP.
• Appoint a regional ACP coordinator to support regional ACP deployment in line with the national ACP policies and the work of the team.
• Negotiate an ongoing budget to support the ACP coordinator/facilitator role.
• Consider how your DHB might support ACP initiatives and the creation of advance care plans (eg, ACP subsidy for primary care).
• Develop clinical pathways to communicate and share processes at a local and regional level (eg, HealthPathways, Map of Medicine, etc).
Downloadable resources and case studies:
• Including ACP in the electronic discharge summary
• ACP subsidy for general practice
• Establishing an ACP mentoring system
• Regional and district ACP integration
• Resource distribution through existing channels
• Implementing electronic ACPs - Case study
• Map of Medicine - developing regional ACP pathway
• Nurse-led ACP clinics in general practice
• Electronic System to share ACP
• Still to come:
– 8 Paper-based system working with St John
– 30 ACP progress note -
Focuses on developing an ACP culture that uses measurement and evaluation tools to determine quality processes and applies them practically for quality improvement.
Actions:
• Collect ACP data.
• Identify local opportunities for ACP improvement and innovation.
• Provide DHB data to the Health Quality & Safety Commission for national measures.
– Contribute to national knowledge on the process and impact of ACP.• Develop pilot projects to implement aspects of ACP, and evaluate using feedback loop processes.
• Use co-design to inform ACP processes and services, and the development of ACP resources.
Downloadable resources and case studies:
• ACP clinical review of plans
• Developing a baseline ACP survey
• Funding for a dedicated ACP facilitator
• Medical Care Guidance (MCG) to support ACP
• Audit of inpatients with ACPs
• Implementing electronic ACPs - Case study
• Still to come:
– 36 Waka model
Embedding
Below are the activities and processes relating to the period when we are moving from creating change to sustaining change. Advance care planning becomes business as usual, an expected activity, and there is entrenched clinical leadership.
The actions listed below relate to ‘embedding’ activities in each of the four quadrants for different parts of the sector. Links to downloadable associated resources and case studies are included.
Note that teams, departments and Te Whatu Ora may be at different stages within and between the various quadrants.
-
Focuses on promoting ACP to the general public and health care sector; normalising future care planning.
Community actions:
Consumers are:
• aware of the need to plan for future care and the importance of sharing what matters to them so it can underpin the planning of their health care
• thinking and talking to whānau and family in the community about ACP
• expecting to have ACP conversations as part of the whole system of care
• acknowledging that death is a natural process that happens to everyone
• receiving care in the place they prefer
• referred to another provider when their needs are more specialised.
Health workforce management actions:
• Management provide appropriate funding to support ACP services and encourage an increase of ACP activity.
Health workforce actions:
• Staff are supported to be ACP ambassadors.
• The health workforce follows advance directives when the situation is relevant. If there are enduring powers of attorney and/or advance care plans, they are enacted and utilised appropriately.
• Staff have the required skills to support conversations and advance care plan development.
• ACP success stories are routinely shared and published across networks.
• ACP promotion and advocacy or patient voice are included in job descriptions.
Downloadable resources and case studies:
• Case study: Integration of ACP into primary care – the Canterbury experience
-
Focuses on increasing the skills and knowledge of the health workforce and consumers.
Community actions:
Consumers are:
• using website and tools
• participating in ACP community meetings
• volunteering to become ACP communicators and trainers
• being empowered through training to co-lead an ACP programme.
Health workforce actions:
• Staff are confident and competent and have integrated ACP into everyday practice. They:
– know how and when to use ACP
– can initiate early conversations
–document all ACP conversations
– participate in team training for support and sustainability, eg, mentoring
– role-model ACP methods and communicate effectively.• Level 1 e-learning is business as usual and there is an expectation all staff will have completed it.
Downloadable resources and case studies:
• ACP education for nursing staff
• Case study: Integration of ACP into primary care – the Canterbury experience
• ACP in undergraduate medical training (Minnesota example)
• Still to come:
– 21 Increasing ACP in the outpatient clinic environment -
Focuses on the systems and processes required to maximise the investment in ACP and training so what is important to consumers is recorded, shared and valued.
Actions:
• Update ACP clinical pathways as and when systems are refined, ie, there is one point of communication with the health workforce.
• ACP is an accepted and expected part of performance appraisal processes.
• Local and national ACP training is advertised through established networks with high demand for training positions within targeted parts of the health workforce.
• Regional networks are established and effective in supporting communication and distribution of information, resources and ideas across DHBs.
• A regional ACP priority workstream is developed.
• Continue working with IT leadership and providers to improve the IT platform.
Downloadable resources and case studies:
• ACP subsidy for general practice
• Establishing an ACP mentoring system
• Regional and district ACP integration
• ACP resource distribution through existing channels
• Integration of ACP into primary care - Case study
• Nurse-led ACP clinics in general practice
• Electronic System to share ACP
• Still to come:
– 8 Paper-based system working with St John
– 30 ACP progress note -
Focuses on developing an ACP culture that uses measurement and evaluation tools to determine quality processes and applies them practically for quality improvement.
Actions:
• Maintain quality cycles and monitor outcome measures (eg, annual evaluation of ACP projects and processes).
• Use collected data and measures to:
– inform ongoing development
– generate reports and presentations for DHB boards, Ministry of Health, Health Quality & Safety Commission, etc.
– inform business cases for further funding approval.• Use collected data and measures for research purposes, such as:
–research articles
– audits.• Continue to adopt co-design processes to inform the development of ACP resources, processes and services.
Downloadable resources and case studies:
• Case study: Integration of ACP into primary care – the Canterbury experience