This guide gives quick ‘how to’ answers to commonly asked questions about completing the paediatric vital sign charts. For more detail, please access the user guide (under the recognition tab).
- How to record oxygen
- Room air
- Low-flow oxygen
- High-flow nasal therapy (high flow)
- CPAP
- Making modification
- Example of modification for chronic condition
- Example of modification for athletic bradycardia
- Whānau concern
- Partial observation
How to record oxygen
Use the ‘respiratory support mode’ key on the back of the chart to indicate the mode.
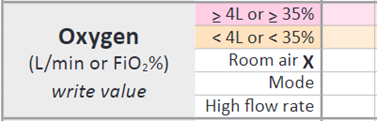
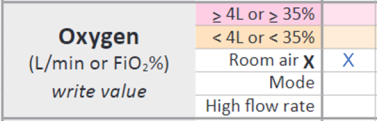
Room air
For tamariki who do not require any form of respiratory support, put an ‘X’ in the ‘room air’ row (see below). This will score ‘0’.
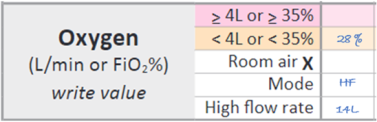
High-flow nasal therapy (high flow)
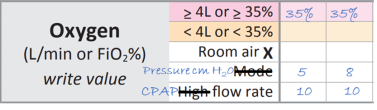
For tamariki on high flow, the FiO2 they need determines their score.
Write the percentage in the orange row if < 35% or the red row if ≥ 35%.
When FiO2 is 21%, write this in the orange row (instead of putting an X in the ‘room air’ row). The score is 2, which recognises that pressure support is still needed even though the FiO2 is low.
The image below shows how to record a tamariki weighing 7 kg on high-flow therapy with an FiO2 requirement of 21%. This will score ‘2’.
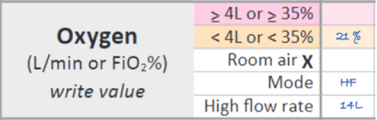
Record the high-flow rate in the ‘high flow rate’ row. This lets clinicians see how many litres per kilo of flow tamariki are receiving.
The image below shows how to record a tamariki weighing 7 kg on high-flow therapy with an FiO2 requirement of 28%. This will score ‘2’.
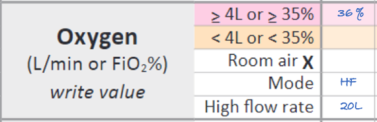
 The image below shows how to record a tamariki weighing 10 kg on high-flow therapy with an FiO2 requirement of 36%. This will score ‘4’.
The image below shows how to record a tamariki weighing 10 kg on high-flow therapy with an FiO2 requirement of 36%. This will score ‘4’.
Low-flow oxygen
For tamariki on low-flow oxygen via a face mask or nasal cannula, the flow rate determines the score.
Write the flow rate in the orange row if < 4 L/min or the red row if ≥ 4 L/min.
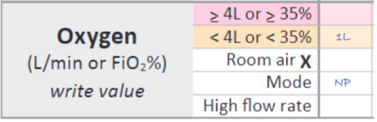
The image below shows how to record a tamariki receiving 1 litre of oxygen via nasal prongs. This will score ‘2’.
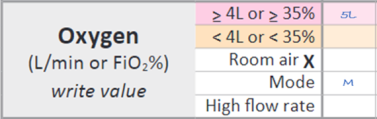
 The image below shows how to record a tamariki receiving 5 litres of oxygen via a mask. This will score ‘4’.
The image below shows how to record a tamariki receiving 5 litres of oxygen via a mask. This will score ‘4’.
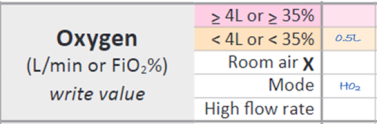
 The image below shows a tamariki receiving 0.5 L/min of humidified oxygen. Scores ‘2’.
The image below shows a tamariki receiving 0.5 L/min of humidified oxygen. Scores ‘2’.
CPAP
If tamariki are receiving CPAP in the ward setting, the PVSC can be adapted to record settings and generate a score. Do this by changing the name of some of the rows to reflect what you need to record on CPAP.
CPAP generates a score based on the FiO2. Record this on the chart in the same way you would for tamariki on high flow.
The positive end expiratory pressure (PEEP) is measured in cm H2O and can be recorded in the ‘mode’ row. Cross out ‘mode’ and write ‘Pressure cm H2O’.
The CPAP flow is measured in litres per minute and can be recorded in the ‘high flow rate’ row. Cross out ‘high’ and write CPAP.
Making modifications
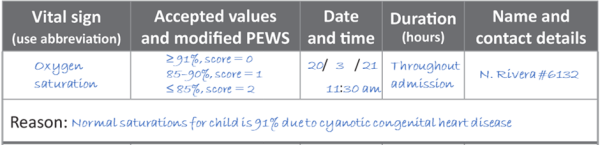
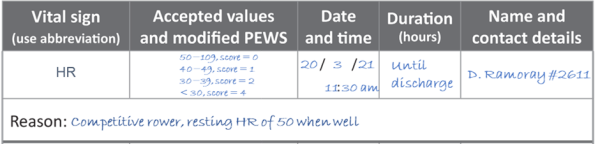
You can modify the PEWS triggers for individual tamariki when chronic disease or abnormal vital sign parameters are present that do not necessarily represent clinical deterioration.
This section of the chart is to capture what is ‘normally abnormal’ for a tamariki. Individual vital sign parameters are altered, not the total PEW score.
When making modifications, consider the clinical risk to the tamariki of normalising an abnormal vital sign. Usually only one parameter should be modified. Making modifications to multiple parameters increases the risk of failing to detect a deterioration.
Document the duration for which modifications apply to ensure there is a timely clinical review.
Check your local policy about who can make modifications. It would be uncommon for modifications to be made without the knowledge and approval of the SMO responsible for the tamariki.
When a new PVSC is used, the modifications will need to be reviewed, redocumented and signed if they are still applicable. Do not just assume modifications remain in place.
Note: When tamariki are unwell and generating high PEW scores, they are likely to remain high until treatment takes effect. In this situation, do not use the modification section to stop escalation. Rather, the review generated by the high PEW score should result in an understanding of why the PEW score is elevated and clear documentation in the patient’s notes of a treatment plan.
This should include specific signs of further deterioration that should be notified, who should be called and a recommended time for the next review.
Having a modification in place should not stop staff calling a clinical emergency if a parameter enters the blue zone or if staff feel a significant deterioration is imminent.
Example of modification for chronic condition
Example of modification for athletic bradycardia
Whānau concern
Y = Yes N = No A = away/asleep/unavailable
This section requires staff to check in with whānau about whether they have any concerns about their tamariki’s condition. Asking regularly gives whānau the opportunity to speak up and voice concern.
Sharing the PVSC with whānau as part of the admission and orientation process, and when completing observations, supports communication, helps understanding and encourages partnership.
If there is concern, mark a ‘Y’ on the chart. Escalation of this concern can occur even if the other observations and the total PEW score are normal. Staff may find that by listening to the concern, explanation or further discussion alleviates it. Document detail in the progress notes, including any action taken because of the concern being raised.
If there is no concern, mark an ‘N’ on the chart.
If whānau members are away/asleep/unavailable, mark an ‘A’ on the chart. This can then act as a reminder for other staff to check in with whānau when they return.
Partial observations
The PEW score total is most accurately assessed with a complete set of vital signs.
Partial observations should be the exception rather than the rule. However, it needs to be acknowledged that sometimes this is neither clinically possible nor desired.
In these circumstances, it is very important that the score is still totalled and recorded in the PEW score total row but add a ‘+’ symbol. This indicates that the score is based on an incomplete set of observations and may in fact be higher.
The escalation pathway is still to be followed regardless of whether it is a partial or full set of observations.

