A surgical site infection investigation tool is a way for health care providers to review and analyse a surgical site infection (SSI) adverse event, to find out why it happened (‘contributing causal factors’) and identify actions to stop it from happening again (improvements in clinical practice). It provides a structured process to follow before making improvements. Printable and electronic versions are at the bottom of this page.
The tool is part of the Health Quality & Safety Commission’s orthopaedic Surgical Site Infection Improvement programme (SSIIP) for light surveillance.
About the investigation tool
This process addresses four basic questions:
- What happened?
- Why did it happen?
- What are the contributing causal factors?
- What can we do to prevent it from happening again?
The investigation tool enables hospitals to identify changes that need to be made to systems through a series of questions that may be linked to increased risk of infection during and following surgery.
Using the investigation tool
The tool can be used to review:
- deep and organ-space SSIs (highest priority)
- superficial SSIs leading to readmission to or delayed discharge from hospital.
The review should be done by someone from the infection prevention and control (IPC) team, surgical services or designee as close as possible to the time the SSI was identified.
Support from leadership is an important part of the investigation because leaders can remove barriers and help drive identified actions.
Steps for reviewing an SSI
Below is a series of steps that are recommended when reviewing an SSI.
Please note it is not a requirement to complete all fields of the investigation tool, it will depend on access to data; the tool is designed to provide prompts for discussion and analysis of contributing causal factors.
- Undertake a preliminary fact-finding review of the patient’s chart using the investigation tool linked below.
- Interview the IPC team/SSI champion and individuals involved in the original procedure to fill in any gaps and identify any practice issues.
- Analyse and identify potential contributing factors.
- Compile a summary of the review and feed this back to relevant teams, eg, IPC team, surgical team, quality and risk team or ward.
- Compare any findings across multiple SSIs.
- Develop a targeted action plan related to any findings.
- Communicate any actions/improvements identified to relevant staff, eg, at department, quality, infection prevention and control committee meetings or morbidity and mortality reviews.
- Recommend and implement solution(s).
- Report the SSI as an adverse event (more information below).
- Include the event on the excel form to be submitted quarterly to the Commission).
National collaboration and support for reducing orthopaedic SSIs
Below is a tool that you can download and compile your findings and actions identified from the investigations.
For questions, please email SSIIP@hqsc.govt.nz.
Alignment with the national adverse events reporting policy
A review of orthopaedic SSIs should align with the national adverse events reporting policy. The table below is an example of how orthopaedic SSIs align with adverse event severity assessment code (SAC) 1‒4 ratings and is for guidance only.
See also the SAC rating and triage tool for adverse event reporting.
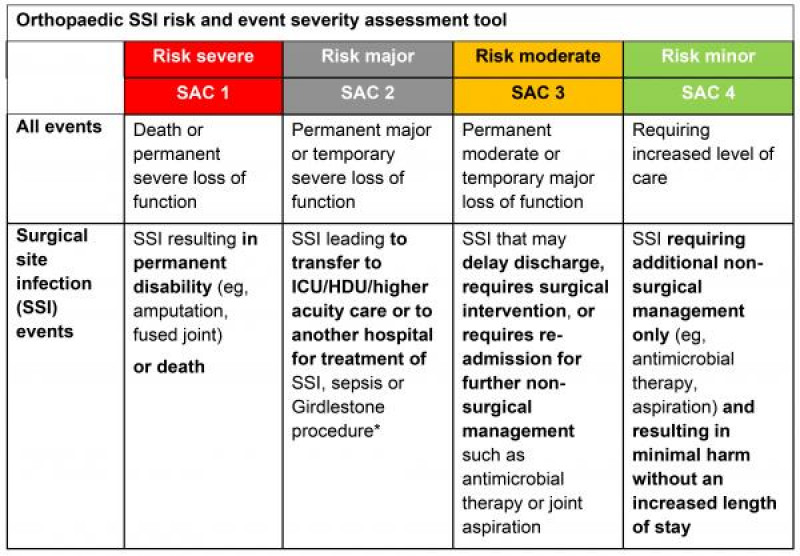
* Girdlestone procedure involves removing part of the ball of the thigh bone or femur, allowing it to fuse with the hip socket (acetabulum) in the straight leg position.
