Partnership delivers wraparound support for diabetes patients
West Coast Primary Health Organisation (PHO) has partnered with Māori health and social services provider, Poutini Waiora, in a project to improve outcomes for targeted Buller Medical Māori and Pacific clients with diabetes.
The holistic care Poutini Waiora provides is primarily mobile, delivering community-based nursing, social services and counselling in whānau homes or other appropriate venues.
The project uses a Whānau Ora model to provide whatever support the patient needs to help them manage their conditions.

West Coast PHO clinical manager, Pauline Ansley, says Poutini Waiora is the ideal partner for the project.
‘When people are struggling, getting their social needs met takes the pressure off, reduces their stress and they’re more inclined to engage with their health.
‘The Poutini Waiora team has been working in partnership with the practice for several years now, seeing their own Māori clients and some from the practice. They have the ability to outreach to those who are not engaging to help improve their access to health care.’
Poutini Waiora provides weekly diabetes clinics at Buller Medical for Māori and Pacific patients. The kaiarataki (health navigator) takes a lead role in the patients’ care by doing height, weight, blood pressure and foot checks and assessing what other support would be useful.
Diabetes and other clinical care is provided by the kaupapa Māori nurse with additional support from Buller Medical’s diabetes nurse specialist and a GP as needed.
The Poutini Waiora team meets with the Buller Medical GP once a week to review each client involved in the project and update their care plans.
‘This also means that Poutini Waiora clients who aren’t enrolled have better access to a GP and are supported to enrol with their general practice.’
While there have been the expected referrals to other services, such as dietitians, Pauline says some of the support provided to the clients has been very personalised.
‘One patient wasn’t taking his medication because he couldn’t afford it and was only eating once a day. The kaiarataki helped him to sort out his financial entitlements with WINZ and introduced him to the community garden where he is now volunteering and is able to take produce home. He was also taken to The Sharing Shed where people donate food and meals.
‘It’s made a big difference and he’s absolutely stoked with everything that being involved in the project has brought him.’
The patients were also surveyed about what would be helpful and said they wanted more information about their medications, diabetes and footcare and what lifestyle programmes were available.
‘We’re producing a medication leaflet to help us introduce medication education for the patient and their whānau so that they understand diabetes better and know what they need to do for themselves. We also did a project to improve the uptake of referrals to the lifestyle programmes.’
The project was undertaken as part of the 2018 Whakakotahi quality improvement programme, which aims to increase quality improvement capability in primary care. Successful providers are supported by the Commission to implement quality improvement projects about an area of patient care that is important to their patients/community and to them as providers. Equity, consumer involvement and integration are key focus areas for Whakakotahi.
The Commission’s primary care programme team supports and mentors participating primary care teams through site visits and group learning events, and a member of each project team is offered a position on the primary care quality improvement facilitator course delivered by Ko Awatea and the Commission's primary care and leadership capability programmes.
Pauline says doing the project under Whakakotahi has given it more authority within the practice. ‘Because the Commission is behind it and the project was accepted through a submission process, there has been more commitment to see it through.’
‘The Commission’s quality improvement advisor, Jane Cullen, has been fantastic, giving us excellent practical support and guidance on using a quality improvement framework. She has also suggested things to try and shared information about what’s worked for the other Whakakotahi projects.’
While the Whakakotahi project is wrapping up, the approach and partnership with Poutini Waiora to improve outcomes for Māori and Pacific clients with diabetes will continue, as will support from the Commission.
‘The goal is to have 90 percent of Māori having their diabetes annual review on time. The difference is using the kaiarataki as part of that process. We’re also trying to keep medications and reviews in sync so people don’t have to come into the practice twice.
‘We’re hoping that, in time, this will model a new way of delivering long-term conditions’ care. This could change the way we do things and we should see the benefits of it in patient outcomes.’
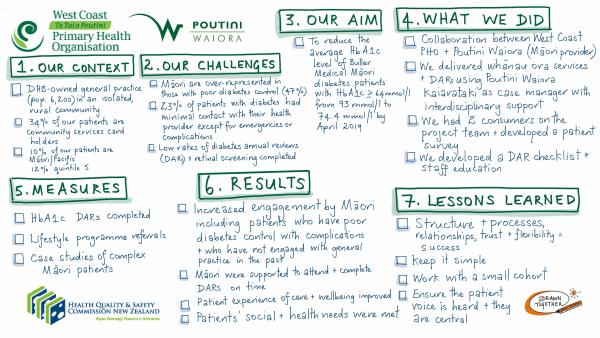
An infographic outlining the project to improve outcomes for targeted Māori and Pacific clients with diabetes. Download a copy of the graphic (1MB, JPG)
