Project inspires quality improvement across West Coast mental health services
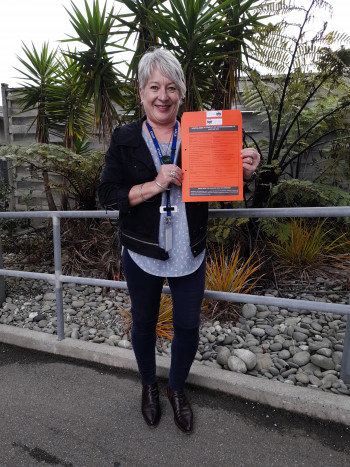
Paula Mason, Nurse manager central MHS, with the new envelope.
Undertaking one quality improvement project relating to seclusion soon highlighted to the West Coast district health board (DHB) mental health and addiction (MHA) services the need for improved processes relating to the coordinated transfer of care of consumers so they and families and whānau receive continued support.
This work by the DHB is part of Te tūhono i ngā manaakitanga, te whakapai ake i ngā whakawhitinga ratonga | Connecting care: Improving service transitions, one of five priority areas for the Health Quality & Safety Commission’s (the Commission’s) national seven-year MHA quality improvement programme.
West Coast DHB nurse manager, central mental health services, Paula Mason, had recently taken up her new role when the DHB began working on the programme’s first priority area, Aukatia te noho punanga: Noho haumanu, tū rangatira mō te tokomaha | Zero seclusion: Safety and dignity for all, and it wasn’t long until the need for further quality improvement was identified in a related area – service transitions.
Paula explains: ‘Once we started the zero seclusion project work, we realised there was so much opportunity for quality improvement across the service, we didn’t know where to start.
‘In the preceding eight months, there had been some horrific events on the ward, including a death, assaults and property damage. The quality and standard of care had to change.
‘It became clear from our zero seclusion project that entry into the service and exit out of it were just as important. Essentially, we combined the two projects and called it “Connecting care to zero seclusion”, because all care needs to be connected.’
The project team included the DHB’s quality manager and mental health services quality facilitator as well as members of the DHB’s consumer council and family and whānau and consumer advisers.
The quality facilitator completed the Commission’s MHA quality improvement facilitator training course delivered through Ko Awatea, Counties Manukau Health.
‘This was really valuable and, along with the support from the Commission, helped us frame up the work we needed to do and make decisions on what to focus on to achieve change,’ says Paula.
‘I also found the regular get-togethers with other DHB MHA quality improvement project teams facilitated by the Commission programme enormously valuable. We picked up so much from hearing what others were doing and thinking about how we could apply what had worked for them to our situation.
‘We put a lot of energy into capturing more feedback through Mārama Real-Time Feedback, a consumer satisfaction survey of consumer and family and whānau experiences of the services they receive in the MHA sector.
‘Our consumer advisor also met with every consumer a month or so after they’d been discharged to ask what they thought could be improved. That feedback helped us change some things, including in the inpatient unit.
‘We developed checklists for admissions and discharges and for inter-DHB transfers to make sure the information was correct, standardised and going to the right people and that the right people had been consulted.’
A new key tool for the inter-DHB transfers is a double-sided envelope to provide a safe way to transfer hard-copy clinical information when staff are escorting consumers between DHBs. Each DHB completes the relevant checklist printed on each side of the envelope.
‘The idea for the envelope came from one used by aged residential care for residents coming into and leaving general hospital care, so we knew the concept already worked and was very popular.’
Paula says quality improvement principles and training are now business as usual for the service and are being applied in other areas.
‘At least 70 percent of our policies and procedures were years out of date, so we’ve been updating those, as well as guidelines for staff, so they’re better resourced. We also have much more robust processes for discharge.
‘In terms of reducing readmission rates, we also looked at improvements we could make to prevent consumers being discharged too early in their journey and to ensure continued care in the community after discharge.
‘Transfers of consumers from the inpatient unit to other DHBs have been static at around six per year. We’ve received positive feedback from receiving DHBs about the transfer envelope, and it has helped to standardise relevant information when we receive consumers back into our care.
‘The Coast is pretty hot on better integration of primary and secondary health services and being more inclusive. We’re now looking at the continuum of care and education around the fact that, when someone comes into mental health care they’ve come from general practice, so they’re already under care. It’s not an “us and them” situation.’
More information about Connecting care: Improving service transitions, including top tips from provider project teams, can be found here.
