Quality improvement project improves medicines access for remote patients
Patients in remote settlements of eastern Bay of Plenty now have better access to timely and accurate medicines, thanks to a quality improvement project undertaken by the Te Whānau-ā-Apanui Community Health Centre in Te Kaha.
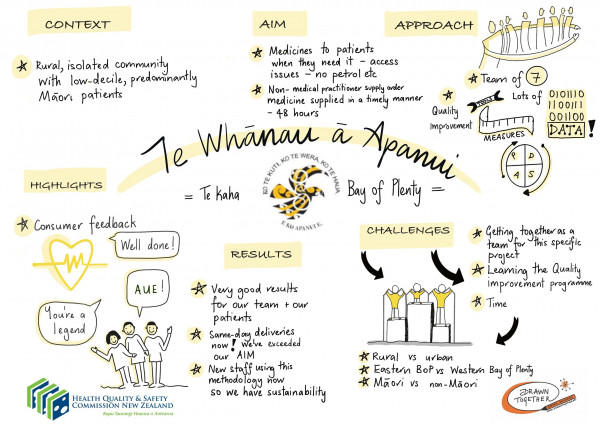
Storyboard summarising the project's aims, approach and outcomes.
The health centre provides general practitioner- and nurse-led clinics for patients living in a 150 km section of winding coastline from Hawai to Pōtaka. While the health centre is at Te Kaha, the nearest pharmacy is an hour’s drive away in Ōpōtiki.
The physical distance is further complicated by a low level of technology infrastructure, often resulting in long delays between patients being prescribed non-urgent medicine and receiving it.
The project aim was to have 90 percent of Te Kaha patients receive their non-urgent medication within 48 hours of it being prescribed, in keeping with expectations for prescriptions generated in Ōpōtiki.
It was one of nine projects from primary care provider teams around the country selected for the Health Quality & Safety Commission’s 2019 Whakakotahi quality improvement programme.
Primary care teams were supported by the Commission to implement quality improvement projects in an area of patient care they wanted to improve that was important to their patients and community, and to them as providers.
All the projects supported the Commission’s three primary care strategic priority areas of equity, integration and consumer engagement. Equity was given greater importance in the Whakakotahi 2019 selection criteria.
A member of each project team was also offered a position on the primary care quality improvement facilitator course delivered by Ko Awatea and the Commission's primary care and leadership and capability building programmes.
The Te Whānau-ā-Apanui Community Health Centre project was one of three in 2019 to benefit from the Commission’s partnership with PHARMAC Te Pātaka Whaioranga to support projects with a medicines access equity focus. These projects received additional support from PHARMAC’s manager access equity.
The health centre is one of only three in the country with the status of ‘a special area’. It operates without a primary health organisation, is funded by Bay of Plenty District Health Board and services are free to all residents within the rohe (area) boundaries.
Around 1,500 predominantly Māori patients are registered, but double that number of patients can be seen casually over the summer holiday period.
Project team supervisor, Dr Emily Gill, says it wasn’t until doing the process mapping part of the quality improvement project that the complicated process of getting the prescription to the pharmacy so that it could be dispensed was fully understood.
‘So many people were involved. It was no wonder things were falling through the cracks.
‘Usually, a prescription is taken to the pharmacy by the patient, either at the time of the appointment, or they’re phoned and asked to pick it up and take it to the pharmacy. This meant everything was in the hands of the patient and it’s simply not practical for a patient to drive an hour or more to drop off their prescription in Ōpōtiki.
‘Doctors were all doing slightly different things with prescriptions, thinking we were being helpful, but it meant prescriptions were going missing.
‘For example, I work remotely and assumed, when I pressed print on my computer, that the prescription was printing in the Te Kaha clinic for reception to then fax it to the pharmacy. But I couldn’t verify that. I was also writing prescriptions late in the evening and putting them in an envelope for a courier to take to the pharmacy, without realising it may not be opened for another couple of days.’
As the project evolved, the health centre’s receptionist, RipekaTe Haara, in discussion with project lead, Kiritahanga Savage, created a filing system to record prescriptions faxed to the pharmacy and a form to help the pharmacy reconcile prescriptions received with medicine delivery.
‘Ripeka would also phone the pharmacy to verify every prescription had been received. This was key to achieving improvement and now all prescriptions go through this process.’
The project team decided to focus its improvement measurement on prescriptions generated for patients seen at the Waihau Bay clinic – a further hour away from Te Kaha and therefore two hours from the pharmacy at Ōpōtiki.
‘They had the most logistical challenges in accessing their medicines because the GP clinic only operates on a Tuesday.
‘There were more errors for this group because we were taking prescriptions back to the main clinic at Te Kaha for processing. However, sometimes we would fax them directly to the pharmacy, but Te Kaha staff didn’t know they’d been faxed.’
Now, every time a prescription is generated, it gets funnelled through one person.
‘This changed the numbers very quickly, with little-to-no issues with Waihau Bay patients receiving their medication within 48 hours of it being prescribed.
‘Patients were part of the measurement process because we phoned them a couple of days after the prescriptions had been written to check they had received their medicine.’
Continual data collection, engaging with, sharing data and getting feedback from patients, iwi representatives, the courier company and the Waihau Bay store where patients can collect medicines couriered by the pharmacy, all made for a more positive end result.
‘We’re still analysing our data, but we know at least 80 percent of Te Kaha patients are now receiving their non-urgent medication within 48 hours of it being prescribed. We have also more than halved the number of medication queries from more than one a day to only one or two per week.’
Dr Gill says the project was important, tailored to the community’s needs and has made a real difference. ‘It was a lot of work, though, and the time needed isn’t built into general practice. It also put more pressure on the pharmacy’s prescription logistics management.’
However, she says staff who were sceptical about the process because of the time involved came away seeing value in it and are now some of the most supportive quality improvement advocates.
‘I don’t think that would have been the case prior to doing our Whakakotahi project, so that’s a huge step. We’re now all very sold on the idea of quality improvement, but we also know we need more support to leverage that.’
