To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Responding when a person raises assisted dying
- Assessment
- Care planning
- Resources for health professionals
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
The New Zealand End of Life Choice Act 2019 gives people who experience unbearable suffering from a terminal illness the option of asking for medical assistance to die. Medically assisted dying involves the person’s doctor or nurse practitioner administering or providing medication to bring on death (Ministry of Health 2022).
Key points
- Assisted dying is not for people who are simply of advanced age or living with disability.
- Whānau/family, welfare guardians or an enduring power of attorney cannot request assisted dying for the person.
- Nurses cannot discuss assisted dying unless the person raises this first.
- Nurses do not have to participate in assisted dying (conscientious objection).
Why this is important
Aged residential care provides services for people with terminal illness. Some residents may ask staff for this service. Check your policy to see if your facility supports this service.
Implications for kaumātua
For Māori, identity is a central element to wellbeing and, as a collectivist culture, ideas of self are entwined with tīpuna (ancestors), whānau/family and community, rather than the emphasis being on the individual’s needs and aspirations (Ministry of Health 2021, p 12).
Tikanga and kawa (Māori cultural customs and traditions) are concepts that are important during the end-of-life process (see the Guide for health professionals caring for kaumātua* | Kupu arataki mō te manaaki kaumātua for more information). Whānau/family have a central role in including and observing them in this process (Malpas et al 2017). Complex and varied whānau/family dynamics, as well as the possibility that assisted dying may conflict with tikanga and kawa, may cause some tension within whānau/family. As a result, health professionals may find this situation challenging to navigate.
Assess the topic of mate whakaahuru (assisted dying) on a case-by-case basis. It is likely that the resident will require whānau/family support for a conversation about assisted dying so, by making time and space for this to happen, you can provide whānau/family-focused, holistic care.
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Responding when a person raises assisted dying
Health professionals working with patients and their whānau/family may be approached by someone wanting to know about assisted dying. These conversations may take the form of a direct request for help to die or a ‘testing of the waters’, using phrases and euphemisms that suggest a wish to discuss the topic further.
Regardless of their personal views, it is important that health professionals are prepared to respond with respect and compassion if someone raises the topic of assisted dying.
The following are two suggested responses.
- Where the person lives independently: ‘This is an important conversation, and I want to help you talk to the best person to support you. May I suggest talking to your general practitioner (GP) or nurse practitioner (NP)?’
- Where the person is in care: ‘Can I arrange for your GP/NP to come and see you?’
The following resources are available on the Te Whatu Ora website. They are designed to support health professionals when responding to an initial request for information. Note, they are not intended to be used to assess a person’s eligibility for assisted dying.
- Responding When a Person Raises Assisted Dying: A handbook for registered health professionals and Responding When a Person Raises Assisted Dying: A conversation guide for registered health professionals
Assessment
To be eligible, the person must meet all the following criteria:
- aged 18 years or over
- a citizen or permanent resident of Aotearoa New Zealand
- suffering from a terminal illness that is likely to end their life within 6 months
- in an advanced state of irreversible decline in physical capability
- experiencing unbearable suffering that cannot be relieved in a manner that the person considers tolerable
- competent to make an informed decision about assisted dying AND retains competence during the whole process, including on the day of administering the medication.
AND two doctors must agree the person is eligible for assisted dying. If one or both doctors think the person may not be competent, a psychiatrist assessment is required.
Care planning
If the person is eligible for assisted dying, the care plan will include deciding:
- date and time of death (which can be any time up to 6 months away)
- place of administering medication
- who else (eg, whānau/family members) may be present
- administration process (self-administered or GP/NP administered).
For an example of a care plan, see www.tewhatuora.govt.nz/assets/For-the-health-sector/Assisted-Dying/Public-information/My-Journey-My-Needs-assisted-dying-care-plan-PDF-353-KB.pdf (PDF, 353 KB).
The person may change their mind about going ahead with assisted dying at any time.
Resources for health professionals
- Te Whatu Ora information for health professionals www.tewhatuora.govt.nz/for-the-health-sector/assisted-dying-service/information-for-health-professionals
- Manatū Hauora Ministry of Health information to print and share with residents and families www.health.govt.nz/our-work/life-stages/assisted-dying-service/assisted-dying-information-public#infosheets
Decision support
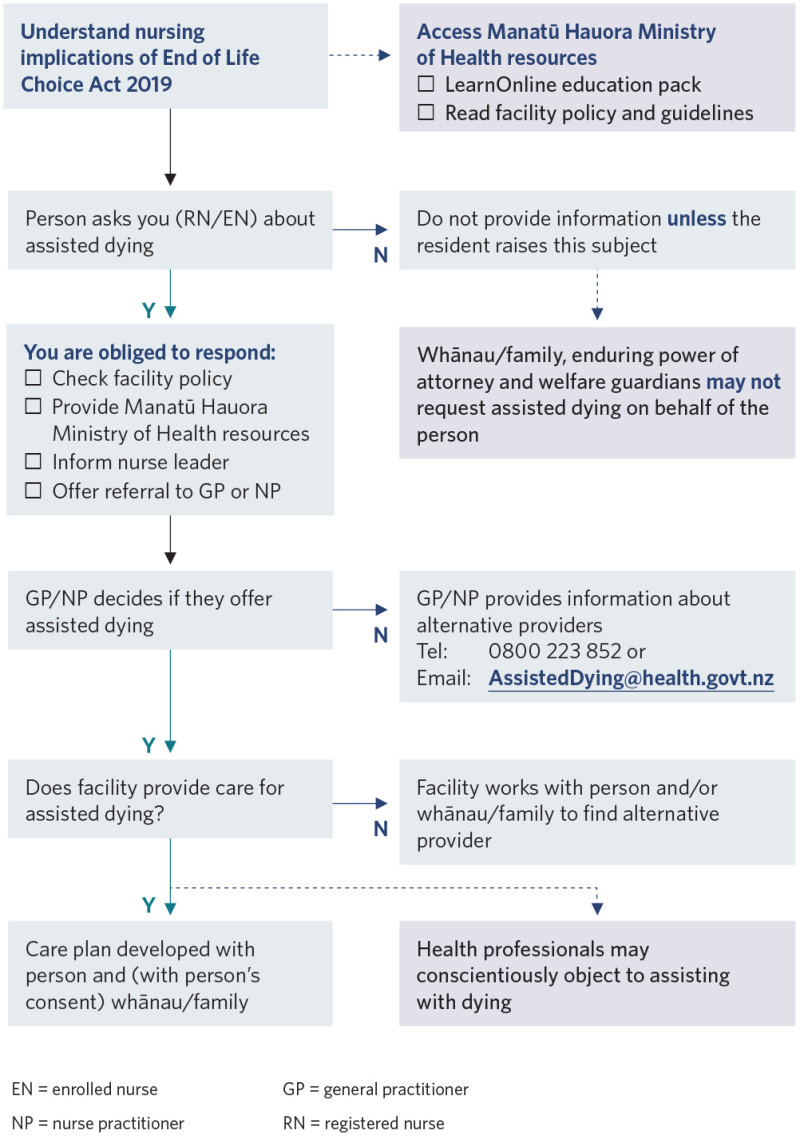
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
Malpas PJ, Anderson A, Jacobs P, et al. 2017. ‘It’s not all just about the dying’: kaumātua Māori attitudes towards physician aid-in dying: a narrative enquiry. Palliative Medicine 31(6): 544–52. DOI: 10.1177/0269216316669921.
Ministry of Health. 2021. Responding when a Person Raises Assisted Dying: A handbook for registered health professionals. Wellington: Ministry of Health.
Ministry of Health. 2022. The End of Life Choice Act 2019. URL: www.health.govt.nz/our-work/life- stages/assisted-dying-service/end-life-choice-act-2019.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
