Chronic obstructive pulmonary disease (COPD) | He mate puru ia auraki (Frailty care guides 2023)
To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Treatment
- Care planning
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
Chronic obstructive pulmonary disease (COPD) is a generic term covering three conditions: chronic bronchitis, emphysema and chronic airflow obstruction, all of which result in limited flow of air through the lung that worsens over time. Unlike asthma, this limitation is not reversible with treatments. Primary symptoms are cough, sputum production, shortness of breath and wheeze (Hancox et al 2021).
Key points
- Exacerbations are common and have a significant mortality risk.
- Long-term COPD causes heart disease: 20–23 percent of people with COPD also have heart failure (Yang et al 2022).
- Long-term COPD affects every aspect of a person’s life.
Why this is important
Severe COPD impacts on every aspect of the person’s life and contributes significantly to the state of frailty. In later states, quality of life often is the priority.
Implications for kaumātua*
Breath and breathing are significant in Māori culture. Te reo Māori has several words for breath, many of which link breath and breathing to te taiao (the natural world) and to Māori creation stories. While these cultural constructs do not change the occurrence, cause or treatments of breathlessness or COPD, it is important to understand them because experiencing breathlessness may contribute to anxiety or wairua (spiritual) unrest (see the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua for more information).
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Assessment
COPD is diagnosed and severity of disease is assessed by symptoms and lung function.
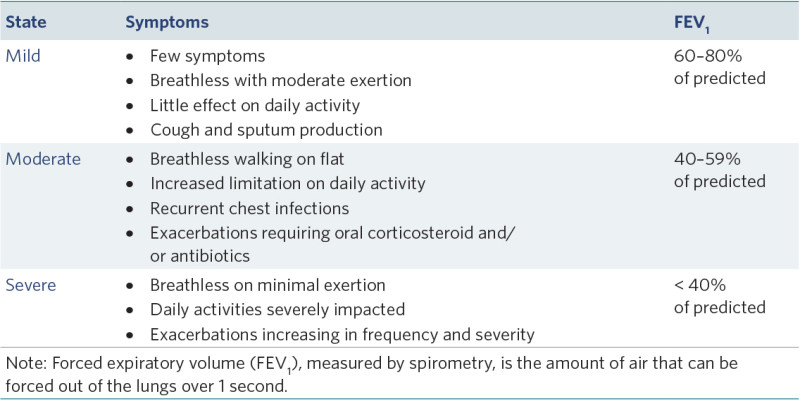
View a higher resolution version of this image in the relevant guide.
Treatment
Non-pharmacological
- Provide support for smoking cessation.
- Provide physical activity and nutritional support (pulmonary rehabilitation where available).
- Provide culturally informed, complementary therapies such as Hikitia te Hā (te ao Māori breathing exercises: www.allright.org.nz/tools/hikitia-te-ha) or waiata (singing), which promote breath control. Whānau/family or a cultural advisor may recommend other therapies.
- Support sputum clearance.
- Support patient and whānau/family to understand the disease process.
- Develop an individual management or action plan (Hancox et al 2022).
- Develop an individual breathlessness plan (Hancox et al 2022).
- Discuss goals of care.
Pharmacological
Routine inhaled medication
Many different inhaled medications for COPD are used in combination for different severity of disease and primary presenting issues. Important nursing roles in managing COPD regimes are:
- inhaler reconciliation – given patients often have multiple inhalers (from different treatment stages), this involves checking that the regimen the patient is following matches the regimen prescribed
- supporting inhaler use, management, technique (including spacer) and infection control
- monitoring and reporting COPD symptoms (because this is a progressive disease so changes in treatment may be needed).
Although treatment may vary between individuals, generally treatment escalates through steps to get maximum control of COPD symptoms.
1. Provide short-acting relief of breathlessness.
a. Choices are short-acting beta2 agonist (SABA) or short-acting muscarinic agonist (SAMA) or a combination (SAMA salbutamol or terbutaline, SAMA ipratropium).
2. Introduce long-acting muscarinic antagonist (LAMA).
a. Examples are tiotropium, glycopyrronium and umeclidinium.
b. SABA can continue.
c. Ipratropium stops – except in emergency situations.
3. Replace LAMA with a combination of LAMA with long-acting beta2 agonist (LABA).
a. Examples are glycopyrronium/indacaterol, umeclidinium/vilanterol and olodaterol/tiotropium.
4. Use inhaled corticosteroids for people with severe disease.
a. Examples include fluticasone and budesonide.
Identifying inhalers
- bpacnz offers an easy-to-follow guide for prescribing decisions and a picture-based inhaler guide that is helpful for staff, patients and whānau/family (bpac.org.nz/copd-tool).
- The New Zealand Respiratory Guidelines provide an inhaler identification chart (www.nzrespiratoryguidelines.co.nz/inhaler-identification.html).
Immunisations
- Annual influenzas
- Pneumococcal vaccination – recommended but not funded (Yang et al 2022)
- COVID-19
Long-term oxygen therapy
- Access through a specialist respiratory service. It is prescribed to improve survival and quality of life by reducing right heart strain. It must be used for at least 16 hours a day at the prescribed dose to be effective. It is delivered by nasal cannula (Barnett et al 2022; Branson 2018).
Care planning
Continuing care for COPD
Severe COPD impacts all aspects of a person’s health and wellness. Help the older person save their breath for doing the things that are most important to them. Care planning includes, but is not limited to, nutrition and hydration, bowel management, skin and bone health, strength and balance, anxiety (particularly panic attacks) and social isolation (Yang et al 2022).
For kaumātua, consider culturally informed holistic interventions including physical activities kapa haka, waiata, karakia and/or te ao Māori breathing exercises (Hikitia te Hā: www.allright.org.nz/tools/hikitia-te-ha). Whānau/family or a cultural advisor may recommend other interventions.
Acute exacerbation
Cases of acute exacerbation always require a general practitioner (GP) or nurse practitioner (NP) review. Symptoms include difficulty breathing, increased sputum production, response to infection and hypoxia. Treatments are aimed at addressing symptoms. They include bronchodilators, corticosteroids and antibiotics and sometimes oxygen therapy, opioids and benzodiazepines (Yang et al 2022).
Short-term emergency oxygen in COPD exacerbation
- Emergency oxygen is only used for cases of low oxygen saturation (SpO2), not simply because the person has a sensation of breathlessness or raised respiratory rate. Oxygen is a prescription medication and must be prescribed.
- When SpO2 is less than 88 percent, use 1–2 litres of oxygen via nasal cannula or 2–4 litres of oxygen via a 24 or 28 percent venturi mask.
- Measure SpO2 frequently and titrate oxygen to reach an SpO2 range of 88–92 percent (Barnett et al 2022; Branson 2018).
Warning: Avoid simple oxygen face masks for oxygen flow rate of less than 5 litres per minute as they put the person at risk of breathing in carbon dioxide (Barnett et al 2022). - This situation requires URGENT medical review (call NP or GP).
Note: Individuals with end-stage disease may vary in their care needs, where they have been assessed by a GP or NP and have a plan in place.
Inhaled bronchodilator
When a bronchodilator is required (eg, salbutamol), a metered dose inhaler and spacer are recommended in the first instance. Some people are established users of an air-driven nebuliser, which may be the required delivery method. Nasal prongs can remain in place during bronchodilator therapy (Barnett et al 2022).
Oxygen-driven nebulisation is not recommended.
Patient positioning
Patients should be allowed to position themselves according to their preference (forcing them to change position will add to stress). Maximising physical support with pillows, the back of a chair or over a bed table, will save energy for breathing (Barnett et al 2022).
Opioids for breathlessness
Regular low-dose oral morphine (< 30 mg daily) can be used to treat breathlessness in advanced COPD. Evidence suggests that once-daily slow-release morphine is ideal.
However, Yang et al (2022) report that patients may prefer immediate-release morphine and recommend low dose with slow up-titration to effect.
Benzodiazepines
Benzodiazepines may be considered as additional support, although evidence for their effectiveness is limited (Yang et al 2022).
Decision support
Routine review
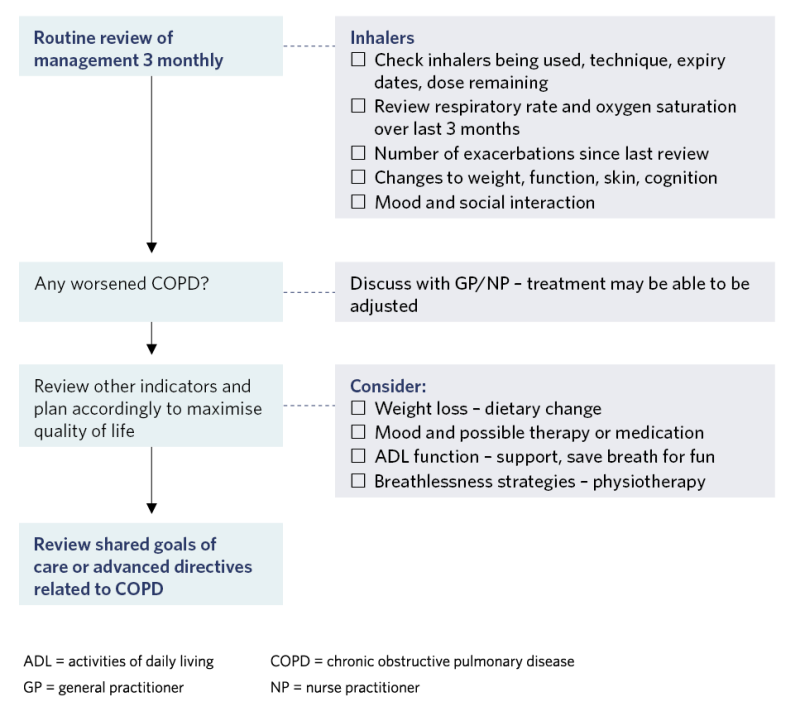
View a higher resolution version of this image in the relevant guide.
Exacerbation COPD
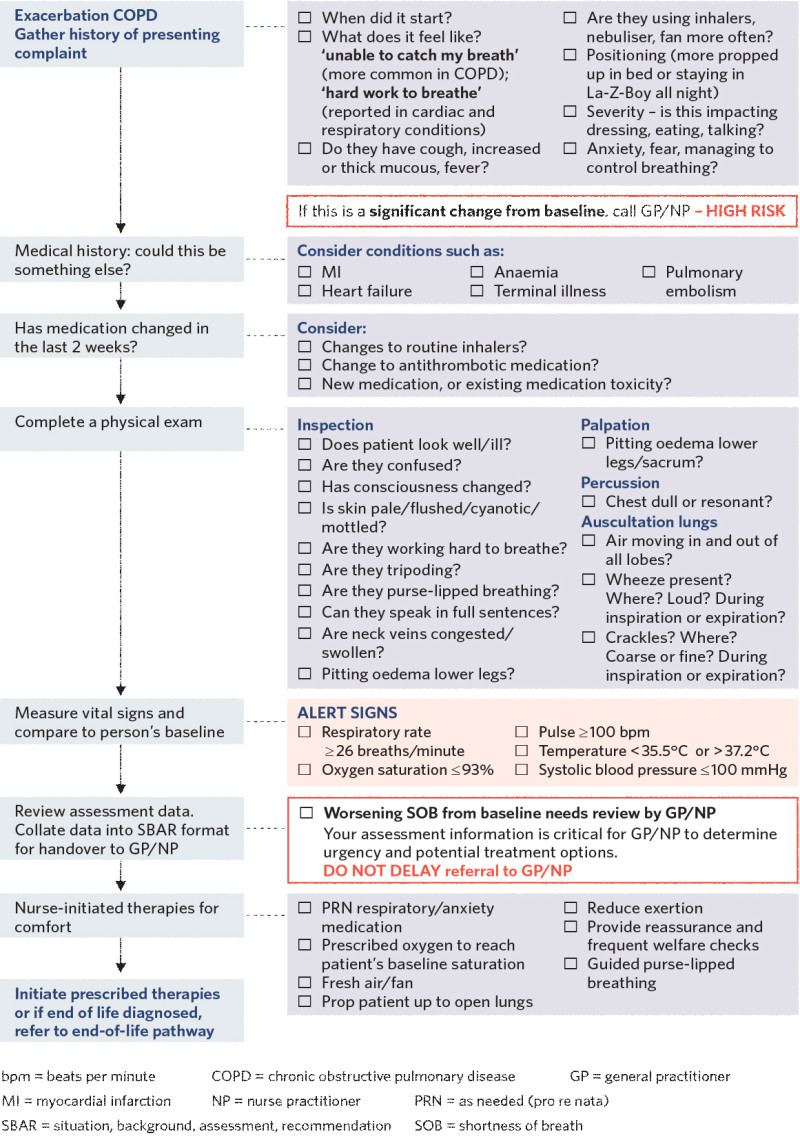
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
Barnett A, Beasley R, Buchan C, et al. 2022. Thoracic Society of Australia and New Zealand Position Statement on Acute Oxygen Use in Adults: ‘Swimming between the flags’. Respirology 27(4): 262–76. DOI: 10.1111/resp.14218.
Branson RD. 2018. Oxygen therapy in COPD. Respiratory Care 63(6): 734–48. DOI: 10.4187/ respcare.06312.
Hancox RJ, Jones S, Baggott C, et al. 2021. New Zealand COPD Guidelines: quick reference guide. New Zealand Medical Journal 134(1530): 76–110. URL: www.nzrespiratoryguidelines.co.nz/copdguidelines.html.
Yang IA, George J, McDonald CF, et al. 2022. The COPD-X Plan: Australian and New Zealand Guidelines for the Management of Chronic Obstructive Pulmonary Disease 2022. Version 2.66. Milton, QLD: Lung Foundation Australia.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
