To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Treatment
- Care planning
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
A fracture is a complete or incomplete disruption in the continuity of the bone structure. When the bone is broken, there is also damage to surrounding soft tissue, muscles, joints, tendons, nerves and blood vessels (Bezella 2021).
Most fractures that occur in residential aged care are ‘fragility fractures’ – that is, a fracture that occurs following low-energy trauma (hip fracture when falling from standing height and vertebral fractures from mild, often unnoticed trauma). The hip, spine and forearm are the most common locations of fragility fractures; however, they also occur in humerus, ribs, tibia (not ankle), pelvis and other femoral locations (International Osteoporosis Foundation 2022).
Key points
- Osteoporosis is the main underlying cause of fragility fractures.
- Those with a cancer history (breast, prostate, lung, melanoma) may experience low- force fracture due to previously undiagnosed metastatic disease.
Why this is important
Hip fractures are the most common osteoporotic fractures in men and women aged 85 years or older (International Osteoporosis Foundation 2022). An estimated 14 to 58 percent of older people die within 1 year of a hip fracture (Schnell et al 2010) and less than half get back to baseline function (Melton 2003).
Implications for kaumātua*
Studies show higher bone density and lower incidence of fractures in those of Polynesian descent, including Māori. Despite this, fractures may still occur in the kaumātua population (Brown et al 2020; Naot et al 2021; Reid et al 1986).
The assessment, treatment and care planning for fractures are the same for kaumātua as for other population groups. However, it may be beneficial to include culturally informed and appealing activities in the exercise regimen. By exploring these options in discussion with the kaumātua and their whānau/family, you can provide holistic, whānau/family-centred care.
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Assessment
- For information on identifying acute fractures, see the decision-support flowchart ‘Acute fracture management‘.
- Bone health: maintaining bone health is the best way to prevent fragility fractures. Osteoporosis New Zealand recommends using the FRAX (Fracture Risk Assessment Tool) or the Garvan ‘Know your bones’ tool to assess a person’s risk of osteoporosis (and risk of osteoporotic fracture).
- FRAX requires a bone mineral density (DEXA) scan for an accurate result. However, anyone who has a fractured bone with minimal trauma is considered to have osteoporosis. The tool is available from the Centre for Metabolic Bone Diseases at www.sheffield.ac.uk/FRAX/tool.aspx?country=23.
- ‘Know Your Bones’ is a web-based (www.knowyourbones.org.au) tool from the Garvan Institute of Medical Research and Healthy Bones Australia. It uses personal details, including risk factors related to health and lifestyle, to estimate fracture risk in the next 5 years. You can download an individual’s report for future reference.
Treatment
Bone health: pharmacological (Best Practice Advocacy Centre New Zealand 2019)
- Bisphosphonates are first-line treatment.
a. Oral bisphosphonates must be given on an empty stomach with a large glass of water, and the person must be able to sit or stand upright for 30 minutes after administration to avoid gastric ulceration.
b. Intravenous bisphosphonates are offered in primary care. They may cause flu-like symptoms.
c. As a group, bisphosphonates must be used with caution in people with renal impairment. (Registered nurses should review renal function with a general practitioner or nurse practitioner in people taking this medication.)
d. Treatment duration: Review of treatment is recommended at 4–5 years, as most evidence comes from studies conducted over 3–5 years.
e. Rare adverse effects include atypical femoral fracture and osteonecrosis of the jaw. Immediately report jaw pain, swelling, lesions, loose teeth or mouth ulceration in people taking bisphosphonates.
- Vitamin D supplementation is recommended for people at risk of vitamin D deficiency. It can be used alone or in combination with bisphosphonates (some bisphosphonate brands already contain vitamin D) (Osteoporosis New Zealand nd).
- Consider deprescribing for all medications that increase the risk of falling and for calcium supplements that are no longer recommended for bone health (New Zealand Formulary 2022).
Bone health: non-pharmacological
- Dietary support may include:
a. protein (to maintain muscle mass) – generally 1.2 g per kg of body weight (bw) per day (as much as 1.5 g/kg/bw/day in malnutrition and reduced to 0.8–1 g/kg/bw/ day in renal failure) (Deutz et al 2014)
b. dietary sources of calcium (Osteoporosis New Zealand nd) – 1,300 mg per day for people aged 70 years and older (one standard yoghurt contains 250 mg calcium)
c. a wide variety of fruit and vegetables.
- Support for exercise (stimulates bone growth and aids muscle strength) may include:
a. designing regular weight-bearing exercise specifically for the individual
b. for kaumātua, considering culturally informed and appealing activities that incorporate exercise. Examples are kapa haka (Māori performing arts) and tītī tōrea (a traditional Māori stick game) and activities that contribute to the community they live in.
- Fracture management: see the decision-support flowchart ‘Acute fracture management‘.
Care planning
Fraction care follow-up management
- Hip fractures will often (not always) need surgical repair.
- Limb fractures are generally immobilised using one of a range of plaster or fibre-glass casts or a range of movement braces.
- Rib fractures are generally left to heal without immobilisation or specific treatment. (Pain management is important to encourage full expansion and contraction of the thorax during breathing.)
General care
- Follow instructions from the acute service. It is important to get specific instructions about weight-bearing status. If in doubt, contact the service for exact instructions.
Fracture care emergencies
Observe for and report emergency complications, in particular:
- deep vein thrombosis and fat emboli (especially in hip, mid-shaft femur and lower leg fractures), with increasing pain, swelling or change in colour, warmth, movement or sensation or sudden-onset shortness of breath
-
acute compartment syndrome (especially in long bone fractures), with increasing pain not relieved by analgesia, sensory changes, pain on passive movement, limb pallor or cyanosis and loss of distal pulse.
Regular limb and cast care (each shift)
- Check limb warmth, colour, movement, sensation, capillary refill time (normal < 2–3 seconds), distal pulses.
- Assess skin integrity at the edges of the cast for signs of friction or rubbing.
- Observe for any of the following: localised burning, itching, swelling, odour or discharge.
- Check for any dents, cracks, soft spots or looseness.
- Consult with medical team before removing back slabs for wound or skin care.
- Always support the casted limb (colour and cuff, sling, pillows).
- Keep cast dry unless waterproof (consider using plastic bag over limb for showering).
- Do not poke things down the cast to relieve an itch.
Range of movement braces
- Follow instructions from the acute service. It is important to get specific instructions about the range of movement allowed and when you can remove the brace. If in doubt, contact the service for exact instructions.
Brace care
- Wash the soft, grey foam with warm soapy water in the washing machine. You can dry the foam in a tumble dryer.
- Keep the brace dry. Cover with a plastic bag in the shower or remove for showering if the provider has given you specific instructions on how to do it.
Rehabilitation
- Immobility associated with a fracture causes significant muscle wastage. The person will need a period of rehabilitation after a fracture. A multidisciplinary rehabilitation plan based on an individual assessment is likely to be needed and to impact all aspects of the comprehensive care plan. A physiotherapist assessment will probably be an important part of the rehabilitation plan.
Decision support
Bone health
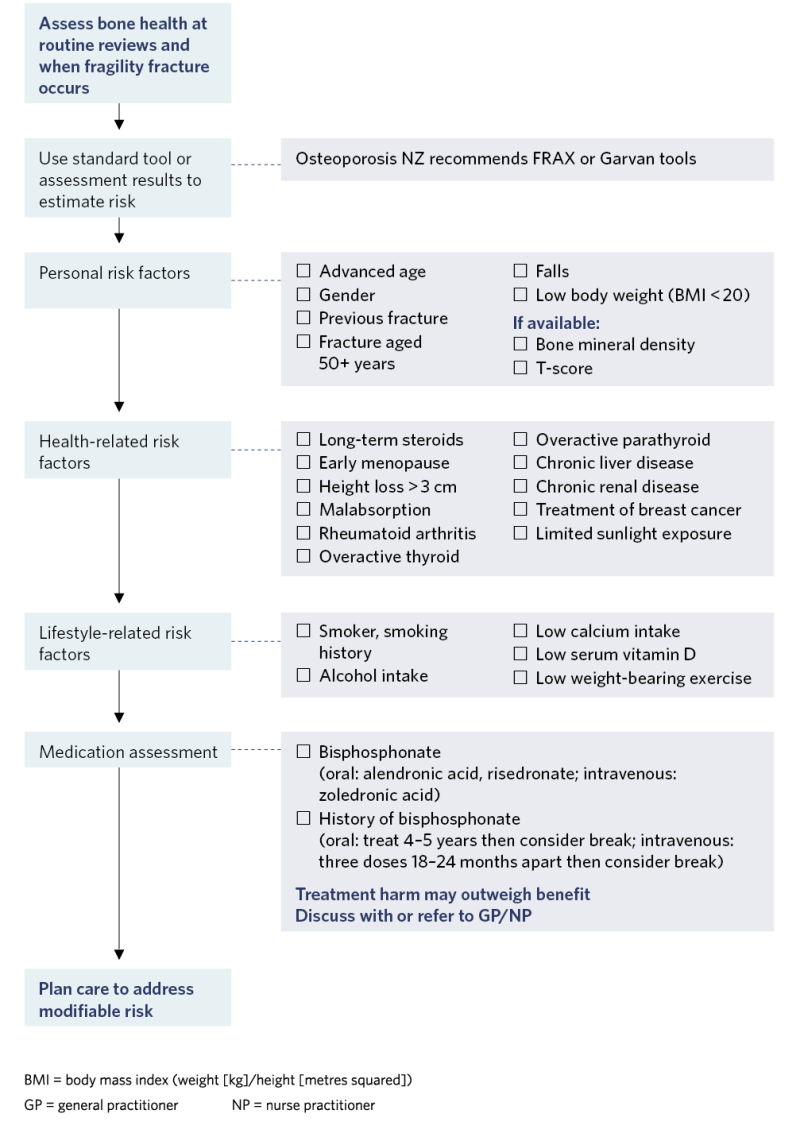
View a higher resolution version of this image in the relevant guide.
Acute fracture management
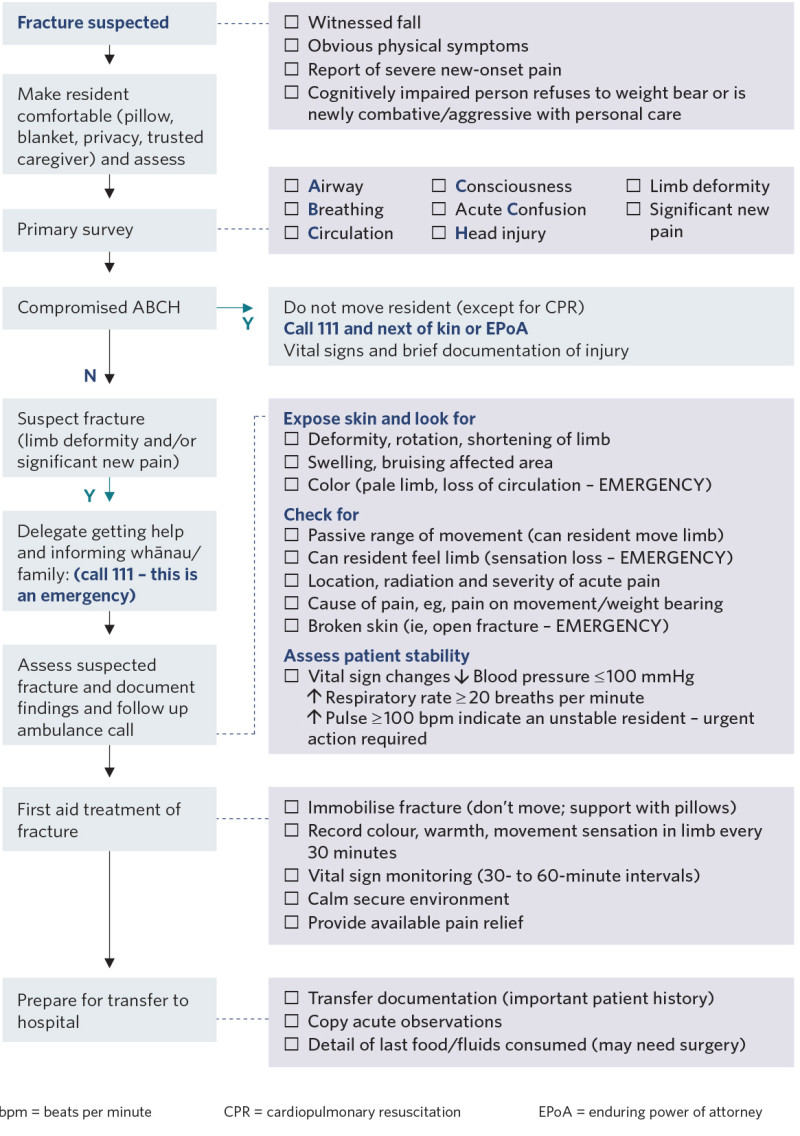
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
Best Practice Advocacy Centre New Zealand. 2019. Bisphosphonates: addressing the duration conundrum. URL: bpac.org.nz/2019/bisphosphonates.aspx.
Bezella M. 2023. Fracture: Study guide for nurses. Nurselabs. URL: nurseslabs.com/fracture.
Brown P, McNeill R, Radwan E, et al. 2020. The Burden of Osteoporosis in New Zealand: 2007–2020. Osteoporosis New Zealand. URL: osteoporosis.org.nz/wp-content/uploads/BONZ_report.pdf.
Deutz NEP, Bauer JM, Barazzoni R, et al. 2014. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clinical Nutrition 33(6): 929–36. DOI: 10.1016/j.clnu.2014.04.007.
International Osteoporosis Foundation. 2022. Fragility fractures. URL: www.osteoporosis.foundation/ health-professionals/fragility-fractures.
Melton LJ. 2003. Adverse outcomes of osteoporotic fractures in the general population. Journal of Bone and Mineral Research 18(6): 1139–41.
Naot D, Bentley J, Macpherson C, et al. 2021. Molecular characterisation of osteoblasts from bone obtained from people of Polynesian and European ancestry undergoing joint replacement surgery. Scientific Reports 11(1): 2428. DOI: 10.1038/s41598-021-81731-5.
New Zealand Formulary. 2022. Osteoporosis. URL: nzf.org.nz/nzf_4006?searchterm=osteoporosis.
Osteoporosis New Zealand. nd. Nutrition. URL: osteoporosis.org.nz/preventing-the-first-fracture/nutrition
Reid IR, Mackie M, Ibbertson HK. 1986. Bone mineral content in Polynesian and white New Zealand women. British Medical Journal (Clinical Research Edition) 292(6535): 1547–8. DOI: 10.1136/bmj.292.6535.1547.
Schnell S, Friedman SM, Medelson DA, et al. 2010. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatric Orthopaedic Surgical Rehabilitation 1(1): 6–14. DOI: 10.1177/2151458510378105.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
