To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Diagnosis
- Supporting the diagnosis
- Treatment
- Infection prevention and control
- Photos to support diagnosis
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
Scabies is a contagious skin infestation of the scabies mite Sarcoptes scabiei variety hominis. It is characterised by an intensely itchy rash that is an allergic reaction to the presence of the mite in the stratum corneum (just under the skin) (Chandler and Fuller 2019).
Key points
- After mating, female mites burrow into the skin and lay two to three eggs every day until death (1 to 2 months). Eggs take 2 to 4 days to hatch. Maturation and ability to reproduce occur in 10–13 days, repeating the lifecycle.
- Mites survive for about 3 days away from a human host.
- Scabies treatments do not kill scabies eggs.
Why this is important
Older adults are the age group most vulnerable to scabies. Scabies rash can take 4 to 6 weeks to develop, during which time infestation can spread by skin-to-skin contact throughout an aged residential care (ARC) setting. Some older people do not develop a classic rash, which delays diagnosis further.
Implications for kaumātua*
To assess for scabies, you need to enter the personal space of a kaumātua, which is considered tapu (sacred, protected). To avoid causing distress and potential damage to tapu and mana (dignity, status, prestige), ask for permission to enter tapu space (Mead 2016). Touching the head is considered very intimate; take particular care to seek permission before doing so.
Kaumātua may experience whakamā (shame, embarrassment) about having scabies, particularly if it is around the groin, genitalia or breasts. For this reason, they may be reluctant to report issues.
Kaumātua and whānau/family may have traditional remedies to help relieve itching and skin irritation. For example, kawakawa balm is known for its antibacterial and anti-inflammatory properties. This guide identifies complementary therapies (additional tools). Explore these on a case-by-case basis and support them where appropriate.
See the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua for more information.
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Assessment
The following are the four main types of scabies (Chandler and Fuller 2019).
- Classical scabies: Most common type, with about 5–15 mites. Intense itchy rash, usually on palms, soles, fingers and toes. Worse when hot (at night and after shower/bath).
- Nodular scabies: Chronic infestation. Clusters of firm nodules under arms and genital areas may persist after successful treatment.
- Crusted (hyper infestation): Thousands of mites. Thick skin scaling, palms, finger webs, soles of feet. Most contagious and causes outbreaks in ARC.
- Complicated: Scabies with secondary skin infection.
Diagnosis
Recommendation: If in any doubt about the diagnosis, refer to a dermatologist for a review.
In an ARC setting, health professionals generally use clinical signs and symptoms to make a diagnosis. Consensus criteria for diagnosis of scabies are available (Engelman et al 2020).
Confirmed scabies – if there is at least one of:
- mites, eggs or faeces on light microscopy of skin samples
- mites, eggs or faeces visualised on an individual, using a high‐powered imaging device
- mites visualised on an individual, using dermoscopy.
Clinical scabies – if there is at least one of:
- scabies burrows
- typical lesions affecting male genitalia
- typical lesions in a typical distribution and itch and positive contact history.
Suspected scabies – if there is at least one of (and if other differentials are less likely):
- typical lesions in a typical distribution and itch or positive contact history
- atypical lesions or atypical distribution and itch and positive contact history.
Supporting the diagnosis (bpacnz 2022; Maguire 2022)
History
Intensely itchy rash on the trunk, limbs or hands, which is worse when hot. In ARC, suspect scabies when a new rash affects two or more people (residents or staff), with the aim of minimising risk of transmission.
Itch is important to diagnosis. However, the onset of itch varies:
- first scabies infestation: 4 to 6 weeks from infestation to itch
- previous scabies: hours to 1 day from infestation to itch (people are sensitised)
- crusted scabies: minimal or no itch.
Itch may also persist for several weeks after treatment.
Examination
People with scabies often scratch skin, and secondary infections and eczema can be present.
-
Hypersensitivity rash: You will find it on trunk and limbs, especially forearms and waist. Polymorphic: scattered erythematous papules (red bumps), pustules and urticated plaques (hive-like). Folliculitis (pimples), impetigo (sores) and eczema (dry or blistered patches) are common in persistent cases of scabies. Long-standing infestation leads to clusters of larger nodules in armpits, groins, genitalia and breasts.
- Burrows: It is best to use dermoscopy (magnification) to find burrows on the wrists, finger web spaces and/or sides and soles of feet. Burrows in any of these locations are diagnostic.
Diagnostic tests:
There is no standard diagnostic test for scabies.
- Classical scabies: Skin scrapings are not recommended because, with so few mites on one person, it is hard to find any (Hewitt et al 2015).
- Crusted scabies: Dermoscopy is recommended. If that is not available, skin scraping can be useful (given thousands of mites are on one person).
Treatment
None of the available treatments is effective against eggs. Treatments applied correctly have the same efficacy (Dressler et al 2016). The logistics of treating a whole ARC facility mean oral medication is more likely to be effective when treating multiple people simultaneously.
Classical scabies – healthy, mobile individuals
- Apply topical 5% permethrin cream or lotion to all skin surfaces.
- Wash off after 8–12 hours.
- Repeat application after 7–10 days (this is enough time for eggs to become mites).
- Treatment requires total skin coverage on all affected people on the same day. In ARC, the logistics required to achieve this may mean treatment failure is a risk and ivermectin may be a more practical treatment (bpacnz 2009).
Classical scabies – debilitated, bed-bound or immobile people
- Administer ivermectin (oral) 200 mcg/kg.
- Repeat after 7–10 days.
Crusted scabies
Recommendation: Consult a dermatologist and skin check everyone in the ARC setting.
- It may be necessary to repeat ivermectin treatment cycles until no burrows are detected.
- It may be necessary to combine permethrin and ivermectin treatments.
Oral ivermectin (Stromectol) dosage:
Available as 3 mg tablets; special authority required
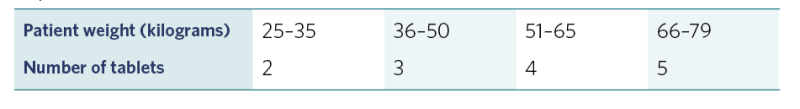
View a higher resolution version of this image in the relevant guide.
Treatment notes
- In ARC, when scabies is diagnosed in any resident or staff member, check the skin of all residents, staff and visitors, at least in the care unit where it is discovered (see Decision Support Tool).
-
Simultaneously treat all affected individuals and their close contacts because some people with scabies may not have developed a rash yet.
Note: Close contacts are people providing direct personal care, people with regular skin contact (eg, hugging, holding hands), intimate contacts and co-habitants.
- In ARC, treatment of residents and staff may be limited to one part of the facility (eg, dementia unit) if residents and staff do not routinely move between care units.
- Coordinating treatment and environmental decontamination is the key to successful eradication of scabies from ARC, even if it takes a few days to develop a plan.
- Public health may be able to help with contact tracing – refer to your local service.
Infection prevention and control
Scabies prevention in ARC
Outbreaks of scabies in ARC are a major headache, so prevention is always preferable. Recommended practice is to check the skin of all new residents in the first day or two of admission and refer skin issues to a general practitioner or nurse practitioner for assessment.
To reduce the risk of a facility-wide outbreak, consider new itchy rashes affecting more than one person (resident or staff) to be an infestation until proven otherwise.
Scabies infestation
Contact precautions: The scabies mite is transmitted by direct skin-to-skin contact with an infested person or contaminated surface. In addition to standard precautions, the following contact precautions are recommended.
- Isolate residents with scabies until they have had their first treatment.
- Direct care staff should wear disposable gloves and long-sleeved gowns when providing personal care for a person with scabies and for handling potentially contaminated clothing, linen and equipment. Continue with these precautions until first treatment (classical scabies) or second treatment (crusted scabies) is completed.
- Laundry staff: Ideally, seal contaminated linen in dissolvable laundry bags and place it in a washing machine without opening the bags . If this is not possible, laundry staff must wear disposable gloves and long-sleeved gowns when handling contaminated linen.
- Limit the number of visitors during treatment. If that is not possible, visitors should also use contact precautions (disposable gloves and long-sleeved gowns) when visiting residents with crusted scabies.
Environmental decontamination
Mites can live in the environment for about 3 days. Killing mites requires extremes of temperature or separating them from the host. Decontamination avoids reinfestation.
Personal environment
On the morning after treatment, decontaminate bedding, towels and curtains (if regularly handled by someone with crusted scabies) by both:
- a hot wash (50°C or 120°F for at least 10 minutes) and
- a hot dry (hottest tumble dryer setting for 20 minutes).
Decontaminate clothing worn immediately before treatment and any items that are regularly handled by the person. Either hot wash and dry as above or if not possible seal dry clothing in a plastic bag and store it at room temperature for 7 days or in a freezer (–20°C) for 12 hours. Note bedding, towels and curtains may also be decontaminated using this method if hot wash is not possible.
Seal cosmetics in a plastic bag for 2 weeks to decontaminate. This timeframe is longer because moist environments prolong mite life (Michigan Department of Community Health 2005).
General environment
Vacuum soft furnishing and carpets in the facility. Where residents’ furnishings are not impervious, cover them for 7 days.
Wipe hard surfaces and residents’ equipment with a solution of detergent and water.
Photos to support diagnosis
from DermNetNZ.org

View a higher resolution version of this image in the relevant guide.
Decision support
Treatment
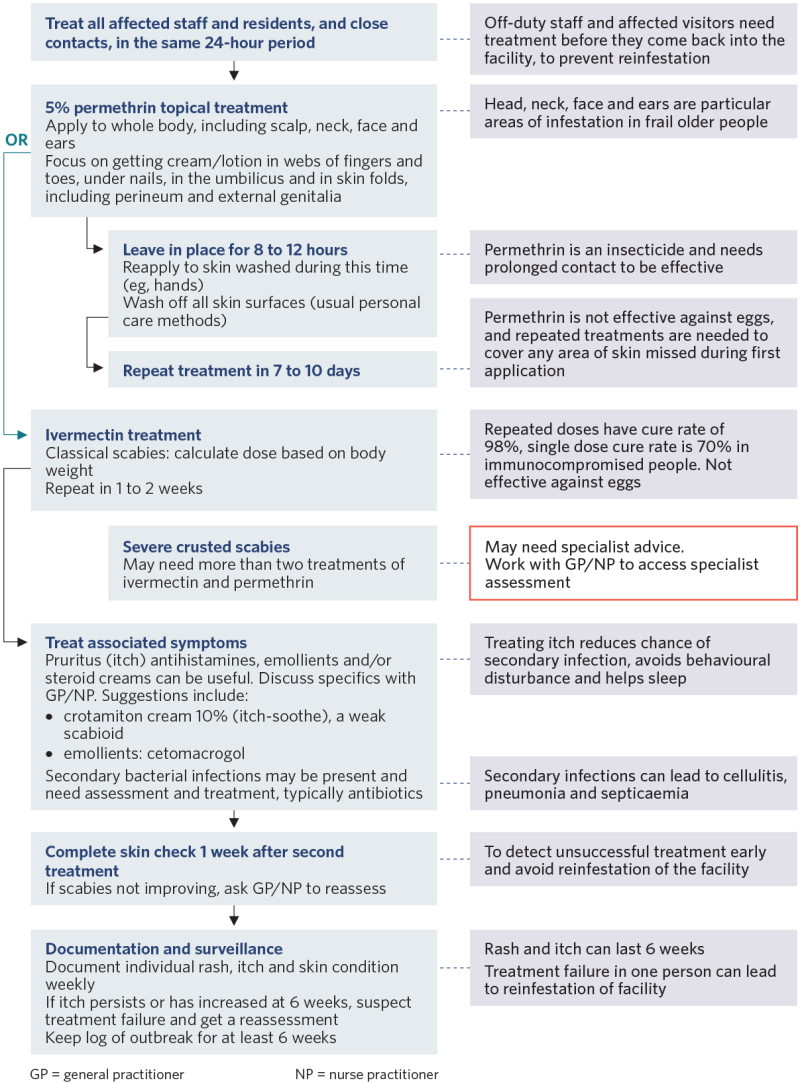
View a higher resolution version of this image in the relevant guide.
Deciding on the extent of treatment
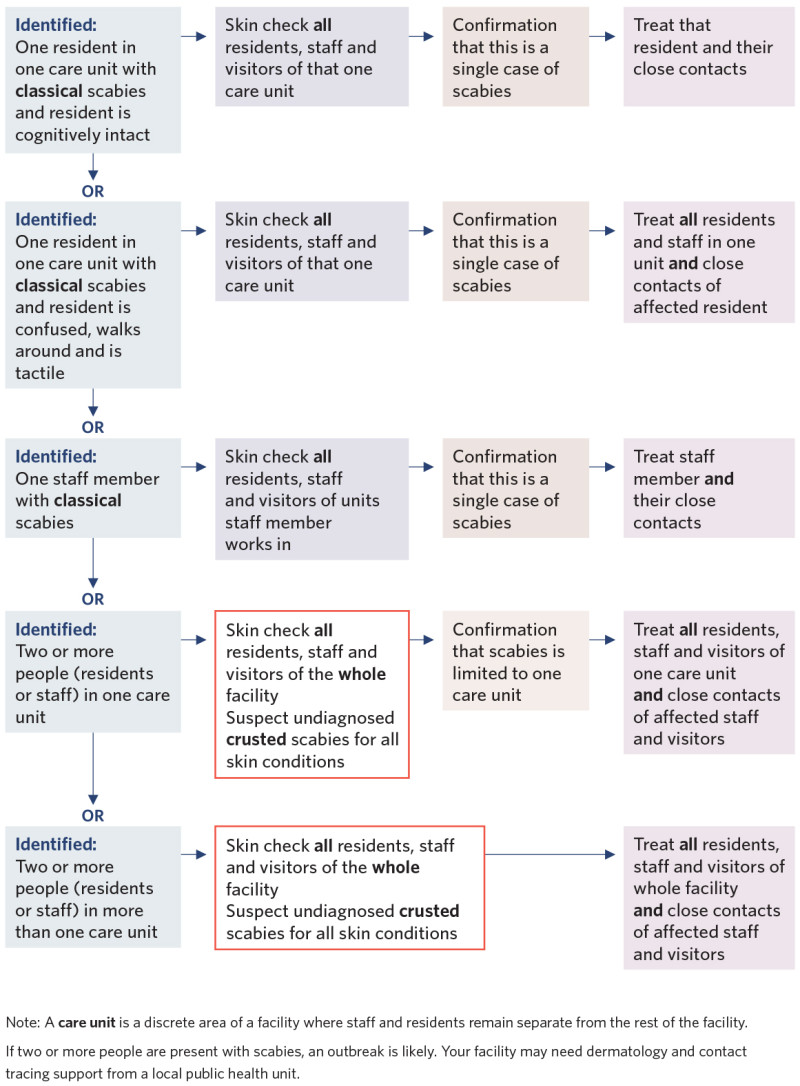
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
bpacnz. 2022. Scabies: Diagnosis and management. Best Practice Advocacy Centre. URL: bpac.org.nz/2022/docs/scabies.pdf.
Chandler DJ, Fuller LC. 2019. A review of scabies: an infestation more than skin deep. Dermatology 235: 70–90. DOI: 10.1159/000495290.
Dressler C, Rosumeck S, Sunderkotter C, et al. 2016. The treatment of scabies: a systematic review of randomised controlled trials. Deutsches Aerzteblatt International 113(45): 757–62. DOI: 10.3238/arztebl.2016.0757.
Engelman D, Yoshizumi J, Hay RJ, et al. 2020. The 2020 International Alliance for the Control of Scabies consensus criteria for the diagnosis of scabies. The British Journal of Dermatology 183(5): 808–20. DOI: 10.1111/bjd.18943.
Hewitt KA, Nalabanda A, Cassell JA. 2015. Scabies outbreaks in residential care homes: factors associated with late recognition, burden and impact. A mixed methods study in England. Epidemiology and Infection 143(7): 1542–51. DOI: 10.1017/S0950268814002143.
Maguire JR. 2022. Scabies. DermNet. URL: www.dermnetnz.org/topics/scabies.
Mead HM. 2016. Tikanga Māori: Living by Māori values. Wellington: Huia Publishers.
Michigan Department of Community Health. 2005. Scabies Prevention and Control Manual. URL: https://bit.ly/46EUIjC.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
