Auckland District Health Board shows zero seclusion is both possible and sustainable

Auckland DHB mental health and addiction co-director Tracy Silva Garay (left) and zero seclusion project lead Pauline McKay
Te Toka Tumai Auckland District Health Board (DHB) has dramatically reduced its rates of seclusion in mental health and addiction (MHA) services. Assaults on staff are down and staff retention is up.
Seclusion is the practice of placing a person experiencing mental distress in a room from which they cannot freely exit. It is traumatic and harmful for consumers, whānau, visitors and health workers alike.
These results are sustainable and can be replicated throughout the country, according to the DHB’s zero seclusion project lead Pauline McKay and MHA co-director Tracy Silva Garay.
‘People say we’ve got a different population in Auckland, but what we have is people. It’s not apples and oranges, it’s people with acute mental health issues,’ Pauline said. ‘It’s about moving from a reactionary space to a preventative space.’
The zero seclusion project
The elimination of seclusion in mental health has been government policy for over a decade. The goal of the Health Quality & Safety Commission (the Commission), in its project titled Zero seclusion: Safety and dignity for all | Aukatia te noho punanga: Noho haumanu, tū rangatira mō te tokomaha, is to continue sector work with DHBs to eliminate seclusion in MHA services. The Commission is working in collaboration with Te Pou (a national workforce centre for MHA and disability in Aotearoa New Zealand) and supporting DHBs to find other ways to manage people in distress, as alternatives to seclusion.
The numbers
Te Toka Tumai Auckland DHB has dropped from 30 seclusion episodes in 2019–2020 to eight in the past 12 months.
At the time of writing, the DHB was 152 days seclusion-free with the last event, a 45-minute seclusion, on 4 February 2021.
The DHB has dropped from 30 seclusion episodes, involving 17 individuals, and adding up to 241.1 hours (July 2019 to June 2020) to eight episodes, involving seven individuals and adding up to 65.3 hours in the past 12 months.
Between July 2019 and June 2020 there were three separate months of zero seclusion events and between July 2020 and June 2021 there were seven months straight of zero seclusion.
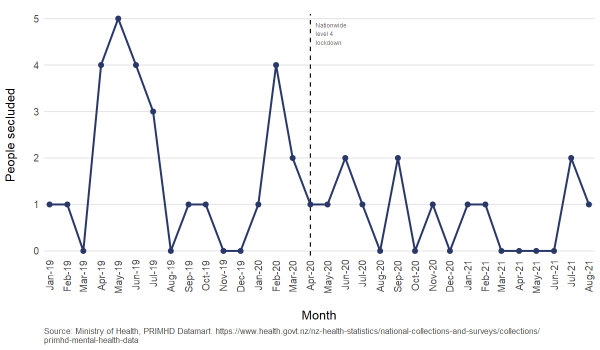
This figure shows the number of people secluded in Auckland DHB’s inpatient mental health units from January 2019 to August 2021. This number has decreased since the peak in May 2019, with the number of months at zero seclusion increasing markedly since August 2020.
Values-based collaboration
Cultural awareness and equity inside the service was an important part of Te Toka Tumai Auckland DHB’s approach, Pauline said. ‘We have had a kaumātua available Monday to Friday and feedback has been that seeing them is very beneficial for Māori. We are also in partnership with the Manukau Institute of Technology to work with Māori and Pacific students on placement. We are actively creating a workplace the reflects our tangata whaiora,’ she said.
The DHB is also working on a rangatahi project. ‘More young people are being admitted and we are not really set up for them. We are doing more quality improvement work in that area. It has opened up so many opportunities.’
Te Toka Tumai Auckland DHB’s approach was a values-based collaboration rather than a fear-based one, Pauline said. ‘It’s the values-based approach that is translateable across the country. It’s been a three-year journey, but the tide is turning.’
Reducing violence
As Te Toka Tumai Auckland DHB has been working towards zero seclusion, there have been fewer incidents of violence – towards both staff and service users – in terms of restraint and seclusion.
During the past year there has been a 30 percent reduction in assaults on staff and a 50 percent reduction in assaults causing harm, Pauline said.
‘When we care, the violence goes down. When we are whānau-centred in our approach, everything else comes with it. Putting the person at the centre makes the world of difference for them and the staff.
At the beginning of the project, community and staff members were worried that the move towards zero seclusion may increase levels of violence. ‘People asked whether other safety measures would be compromised to achieve this reduction, but they have seen it work over time, and the violence drop. We acknowledge that no assault is okay and are working hard to continue to reduce these incidents,’ Pauline said.
Listening to the voices of the people secluded
The Te Toka Tumai Auckland DHB zero seclusion team wants to learn from people who have been secluded. They plan to talk to the eight people secluded in the past year to see what could have made a difference in their care. ‘We need to hear from those eight voices to see how we can respond to our community in the best way possible,’ Pauline said.
The DHB is aiming for more and more months of zero seclusion incidents and decommissioning the last seclusion room is the ultimate goal, she said.
The team meets fortnightly to continue to work towards eliminating the practice of seclusion.
‘We are part of regional and national groups discussing shared challenges – such as methamphetamine intoxication. And we will be partnering with others on any approaches developed.’
Nurses are our allies
Te Toka Tumai Auckland DHB has a strong focus on supporting its nursing staff, said Tracy Silva Garay.
She particularly acknowledged the hard work of the team at Te Whetu Tawera, the DHB’s acute mental health unit for adults. ‘We will continue to support the nursing team to reach forward with compassion and empathy to our most vulnerable, even during heightened distress.’
Nurses have shown leadership throughout the zero seclusion process, she said. ‘We have really strong nursing leadership – people who understand the business, people who come from a place of knowledge. People come in [to MHA services] and are part of an environment where the nurses support them, so we want to support our nurses.’
Mindfulness-based sessions for staff after handover have generated particularly positive feedback, she said. ‘We need to look after nurses’ mental health as well. Mindfulness helps them start their shift in the right state of mind. It helps with the handover as they are less hyped about the information they are receiving if there were any issues before their shift. They are able to re-centre. I truly believe the therapeutic focus on interactions has helped the unit recruit and retain staff,’ she said.
Good things take time
Moving towards zero seclusion has been a long-term project that is coming to fruition, Tracy said.
‘We took a longer time to decide what we were going to do and there were plenty of difficult discussions from the outset before we were all on the same page. The upside was, once we were there, we were certain. Once our vision was set, it never changed.
‘When new people come in, they are coming into a culture that is already set. They know what our intent is. We care for our staff, the people who use our services and their whānau. If you are going to join us, this is what you are joining.’
The challenges
According to Pauline and Tracy, most seclusions happen in the first 24 hours of admission, usually on entry, when people are acutely unwell. Issues around patient flow and a shortage of adult beds exacerbate this, Tracy said. ‘We’ll have two free beds and five people needing beds. We’re at 100 percent occupancy each day.’
Sector and police liaison is something Tracy would also like to see happen more. ‘Seclusion isn’t just something that happens at a point in time; there’s a path to it and we need to look at that too.’
Methamphetamine is a big issue that all DHBs are grappling with. ‘Meth or another substance intoxication was involved in all eight seclusions,’ she said.
More information
For more information on the Commission’s zero seclusion project, please visit our website:
