National decrease in seclusion rates in inpatient mental health units – particularly among Māori and Pacific peoples
Recent data from the Health Quality & Safety Commission (the Commission) shows a national decrease in seclusion rates in inpatient mental health units, including a substantial drop for Māori and Pacific peoples.
Seclusion is the practice of placing a person experiencing mental distress in a room from which they cannot freely exit. It is traumatic and harmful for the person, their whānau, visitors and health workers alike.
The Commission’s Zero seclusion: safety and dignity for all | Aukatia te noho punanga: noho haumanu, tū rangatira mō te tokomaha project team has worked in collaboration with district health boards (DHBs) to find alternatives to seclusion for people who are experiencing distress. The project began in 2019 and is now seeing the positive effects of decreased seclusion rates.
Seclusion rates increased from 2015 to 2019, but have since stabilised and by late 2020, the number of people experiencing a seclusion event had decreased.
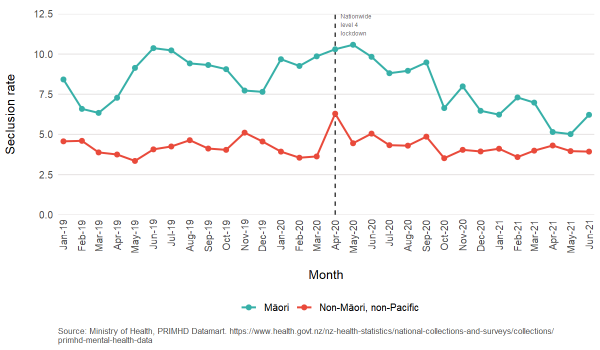
Seclusion rates for Māori have recently been decreasing at a faster pace than for non-Māori non-Pacific, shrinking the equity gap between the two population groups.
Bending the curve at a national level
Rate of Māori and non-Māori, non-Pacific mental health inpatients secluded, Aotearoa New Zealand, 2019–21
Commission mental health and addiction (MHA) quality improvement programme clinical lead Dr Clive Bensemann said the current data showed a bend in the curve in seclusion numbers for the first time since since 2015.
‘At a national level we have bent the curve in seclusion numbers and another quarter’s worth of data will make it clear if this change is a sustained, significant reduction,’ he said.
These results are reflected in many DHBs across the motu, with Auckland, Whanganui, South Canterbury, West Coast and Lakes DHBs all seeing a reduction in seclusion rates and, at times, reaching and sustaining zero seclusion.
‘These encouraging results in both increased equity and overall reduction in seclusion rates, confirm what we have been learning from case studies,’ said Dr Bensemann.
More about the zero seclusion project
The elimination of seclusion in mental health has been government policy for over a decade. The Commission’s goal, through its zero seclusion project, is to continue sector work with DHBs to eliminate seclusion in MHA services. It aims to improve the experience of care for people who are experiencing distress by reducing seclusion rates in all acute in MHA settings by 50 percent by 1 June 2022, contributing towards the goal of zero seclusion.
This work is being done in collaboration with Te Pou (a national workforce centre for mental health, addiction and disability in Aotearoa New Zealand), which is supporting DHBs to find other ways to manage people in distress, as alternatives to seclusion.
For more information, visit our zero seclusion project page.
Increasing equity for Māori and their whānau
In 2018–19 Māori were most likely to be secluded. Since September 2020 there has been a notable reduction in both the seclusion rate for Māori (from 9.5 percent in September 2020 to 6.2 percent in June 2021) and the difference between the seclusion rate for Māori and non-Māori non-Pacific (from 4.8 percent in September 2020 to 2.3 percent in June 2021).
MHA quality improvement programme Māori advisory group (MAG) chair Wi Keelan says where there are strong, meaningful partnerships with Māori within DHBs and the community, seclusion rates have reduced. This also includes strong Māori leadership within DHBs.
‘Including the principles of Te Tiriti o Waitangi in everything we do is essential to achieving and normalising equity within our nation’s mental health and addiction services. Significant progress has been determined by services engaging with kaupapa Māori services, and kaimahi Māori at every level,’ he said.
‘Where there are solid and meaningful partnerships in the care of Māori and their whānau, including shared care arrangements between the DHB and iwi Māori health providers, seclusion rates and inequity have reduced.’
Work towards zero seclusion begins before a person is admitted to an inpatient unit, Matua Keelan says.
‘We have to do better and engage with our whānau in their homes and in their communities… actually going out there and working with them to prevent admissions to acute mental health units in the first place,’ he said.
The zero seclusion project advocates for the incorporation of kaupapa Māori approaches and is currently developing a cultural kete to help further support DHBs, he said.
‘Where you have a reduction in seclusion, you have more compassion, more kindness, more talking, more storytelling.’
Zero seclusion in action at DHBs
Te Toka Tumai | Auckland DHB has managed to dramatically reduce its rates of seclusion in MHA services. Assaults on staff are down and staff retention is up.
Against a background of evidence, including a national seclusion rate for Māori of 16.2 percent in 2020, and a Pacific rate of seclusion of 12.6 percent in the same period, Te Toka Tumai | Auckland DHB has been able to stay at zero or close to the elimination target over the past three years.
Read more about this here: Auckland District Health Board shows zero seclusion is both possible and sustainable.
Keep an eye out for more in our series about DHBs making zero seclusion sustainable.
Seclusion and COVID-19
The highest seclusion rates occurred during the initial COVID-19 lockdown in 2020. This is likely to be a statistical anomaly. The number of people secluded remained constant, but admissions fell dramatically, leading to a spike in the seclusion per admission rate (no such spike occurs if we measure seclusions against population rather than admissions).
The cultural kete and clinical bundle
The zero seclusion team is producing a cultural kete and clinical bundle to further support DHBs in the elimination of seclusion. These will be released later this year.
The cultural kete is being developed by the Māori advisory group, working with the Commission’s MHA quality improvement programme team, the zero seclusion champions group and DHB project teams. It aims to give people and whānau better access to a broader range of services than is available currently and greater choice in the types of support they receive.
The kete will gather a list of cultural interventions, some of which are already in use by project teams, and show anecdotal evidence of success. These interventions will be identified, defined and made available to DHB MHA services, people experiencing mental illness and their whānau, iwi Māori providers and other non-governmental organisation partners.
‘The holistic interventions envisaged in the kete will enhance existing clinical therapies and, over time, the effectiveness of this approach will be tested through co-design and the science of the Institute for Healthcare Improvement’s quality improvement methodology,’ Matua Keelan said.
This approach is expected to expand access and choice, include holistic tools, promote whānau engagement and improve Māori community involvement and resilience, thus preventing and eventually eliminating the need for seclusion practice.
The clinical bundle has been developed by the Commission team working with the zero seclusion champions group and project teams. The bundle describes the changes that, when implemented together, will reduce the use of seclusion and move services more rapidly towards elimination, based on evidence from the literature and practice-based evidence from project teams.
‘The cultural kete and clinical bundle complement and inform each other in the interventions they describe,’ said clinical lead Dr Bensemann. ‘Used together they will have the greatest impact.’
For more information see:
