To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Treatment
- Care planning
- Further resources
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
Heart failure is a complex clinical syndrome, where changes to the structure or function of the heart reduce cardiac output. With or without treatment, heart failure progresses over time so older adults are more at risk than their younger counterparts (bpacnz 2022).
Key points
- Overall, heart failure affects at least 10 percent of people aged over 70 years. Within this group, about 50 percent die within 5 years of diagnosis.
- Up to a third of people living in residential care have heart failure (Daamen et al 2015).
- Māori and Pacific peoples experience an earlier onset of heart failure and a higher rate of morbidity and mortality than other New Zealand ethnic groups (bpacnz 2022).
Why this is important
Heart failure is both chronic and progressive. However, treatment can relieve symptoms and improve function and quality of life (Daamen et al 2016). Understanding disease stage supports conversations about treatment and care options. Management of heart failure can be complicated by frailty and other chronic conditions, such as diabetes and chronic respiratory disease (Riley 2015).
Implications for kaumātua*
The burden of cardiovascular disease (CVD) disproportionately affects Māori compared with New Zealand Europeans (Ministry of Health 2018). The reasons are related to ongoing inequities in health and in experiences of social determinants of health (Miner-Williams 2017; Selak et al 2020). Due to the higher incidence of CVD in Māori, it is likely that there will be kaumātua in aged residential care who have heart failure. Providing them with appropriate care is vital.
A Māori view of health is holistic. When caring for kaumātua with heart failure, it is important to consider care from this perspective, rather than focusing solely on the disease of heart failure. A holistic approach takes account of the person’s spiritual and emotional wellbeing and includes their whānau/family.
The following are aspects to consider in your approach to care.
- Kaumātua and whānau/family may see symptoms associated with heart failure as a normal or expected part of ageing. If they do, it is essential to give them all the information they need to fully participate and engage in treatment and ongoing management.
- For effective management of CVD, health professionals must have a trusting relationship with kaumātua and whānau/family (bpacnz 2008; Kerr et al 2010).
- Whakawhanaungatanga (building meaningful connections) is critical in establishing these relationships. See the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua for more information.
Whānau/family can be a useful source of valuable, culturally informed (mana-enhancing) interventions as they are invested in the health and wellbeing of their loved one. Involve them in care planning wherever possible.
Assessment
Nursing assessment of heart failure includes identifying potential new cases, maximising the health of those with heart failure and responding to acute exacerbations.
Identifying new heart failure
- New-onset heart failure can be difficult to identify because classic symptoms, such as dyspnoea, fatigue and reduced exercise tolerance can be caused by other conditions (bpacnz 2022).
- People with heart failure are more likely to have a history of cardiac disease, fatigue, irregular heart rate, oedema in lower limbs, rapid weight gain and breathlessness when lying flat (orthopnoea) or that causes sudden waking from sleep (paroxysmal nocturnal dyspnoea) (Daamen et al 2015).
- ANEWLEAF is a tool that can help identify acute exacerbation of heart failure if that occurs as part of a new heart failure diagnosis or as a result of unmanaged disease (Heckman et al 2018).
A – Agitation/anxiety (especially if new)
N – Nights bad: trouble breathing, urinating more
E – Oedema (swelling in which you can leave a fingerprint indentation)
W – Weight gain (from water retention)
L – Light-headed, dizzy
E – Extreme trouble breathing when lying flat
A – Abdomen bloated, abdominal pain, not hungry
F – Fatigue, tired - The most common primary care diagnostic test for heart failure is N-terminal pro-brain natriuretic peptide (NT-ProBNP). In people aged 75 years and over, a level of more than 210 pmol/L (1,800 pg/ml) makes heart failure likely (bpacnz 2022).
Identifying an acute exacerbation of heart failure**
- Use the tool ANEWLEAF (see above).
Other signs
-
Look for evidence of fluid overload, pitting lower limb and/or sacral oedema. Listen for audible ‘wet’ breath sounds (Riley 2015). Check the person’s weight: an increase of > 2.5 kg in 1 week or > 1–2 kg in 24 hours is significant.
- Measure vital signs. Most people will have normal or high blood pressure in the early stages of an acute exacerbation (Mebazaa et al 2015).
- Shortness of breath is a key sign – see the first table below.
**Some heart failure patients present with chest pain or syncope. See the guides to Acute deterioration | Te tipuheke tārū or Syncope and collapse | Tīrehe.
Breathlessness in heart failure (adapted from Mebazaa et al 2015)
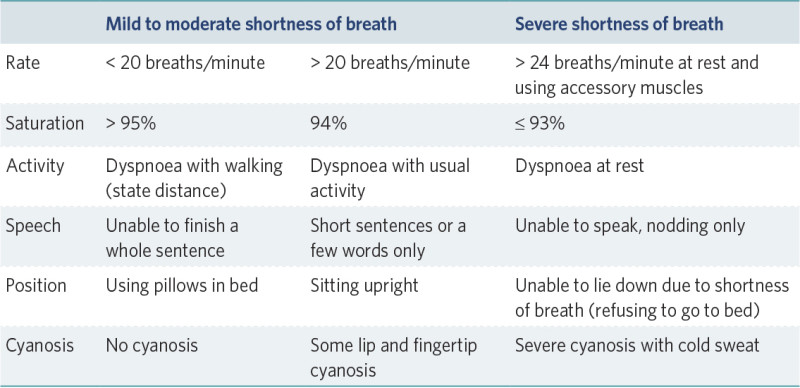
View a higher resolution version of this image in the relevant guide.
Staging diagnosed heart failure
- Disease staging reference: New York Heart Association (NYHA) classification
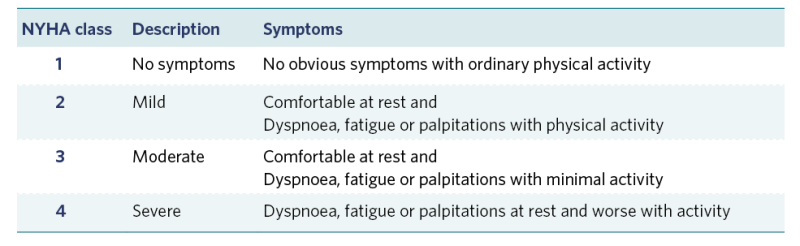
View a higher resolution version of this image in the relevant guide.
- The definition of advanced heart failure from the American College of Cardiology Foundation and American Heart Association is:
- more than two hospitalisations in 1 year
- progressive deterioration in renal function
- unintended weight loss (cardiac cachexia)
- unable to tolerate angiotensin-converting enzyme (ACE) inhibitors or beta-blockers because of hypotension and/or worsening renal function
- needing more than 160 mg of furosemide (or equivalent) daily
- hyponatraemia.
- Although the mortality rate with heart failure is high, no particular tool is any better at estimating life expectancy than clinical experience. Conversations about advance care planning or shared goals of care are part of caring for someone with heart failure.
Treatment
Pharmacological
The mainstay of treatment is pharmacological. Use a loop diuretic to improve symptoms of fluid overload and an ACE inhibitor, a beta-blocker and spironolactone to decrease the chance of mortality and hospitalisation. Individuals will vary in their response to medicines; however, provided there are no contraindications, medications are usually titrated to the most effective dose (Atherton et al 2018).
Monitoring for medication benefits and potential harms
- Weigh daily, ideally first thing in the morning and the same time every day. If the person gains > 1–2 kg in 24 hours or > 2.5 kg in 1 week, they require general practitioner or nurse practitioner review.
- If diuretic has been changed, weigh daily. Review and report results against target weight and timeframe. Alert prescriber when targets are either not met or exceeded.
- Review laboratory results. Look for low sodium, low haemoglobin and decreasing estimated glomerular filtration rate (Atherton et al 2018).
- Be alert for signs and symptoms of gout (Atherton et al 2018).
- Be alert for heart failure symptoms when any medication is changed (eg, corticosteroids increase the risk of fluid overload and antidepressants can worsen hyponatraemia).
Fluid balance
- To help fluid management, restricting fluid to 1.5 L per day is common. Also recommended is to limit sodium intake to no more than 2 g per day (Atherton et al 2018).
General health
- All treatments for frailty are relevant to this group.
Care planning
Heart failure is a progressive chronic condition that worsens frailty. Interventions aimed at delaying or improving symptoms of frailty (physical activity, nutrition, social care), along with medication management, apply to this group.
Further resources
Chronic Disease Management in Long-term Care: Heart failure. Provincial Geriatrics Leadership Ontario webinar. URL: rgps.on.ca/resources/chronic-disease-management-in-long-term-care-heart-failure.
Decision support
Diuretic management
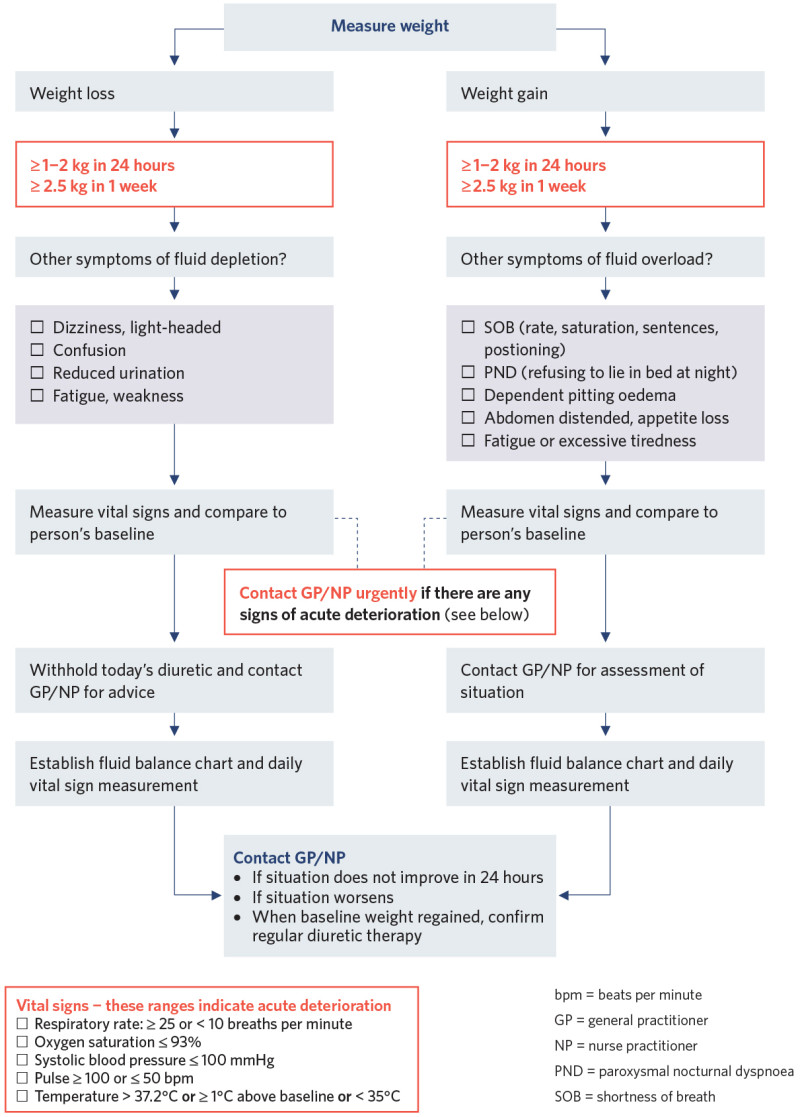
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
Atherton J, Sindone A, De Pasquale CG, et al. 2018. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of heart failure 2018. Medical Journal of Australia 209(8): 363–9. DOI: 10.5694/mja18.00647.
bpacnz. 2008. Cardiovascular disease and diabetes in Māori. Best Practice Journal 13: 15–19. URL: bpac.org.nz/bpj/2008/may/docs/bpj13_cardio_pages_15-19.pdf.
bpacnz. 2022. Addressing heart failure in primary care. URL: bpac.org.nz/2022/heart-failure.aspx.
Daamen MAMJ, Hamers JPH, Gorgels APM, et al. 2015. Heart failure in nursing home residents: a cross-sectional study to determine the prevalence and clinical characteristics. BMC Geriatrics 15: 167. DOI: 10.1186/s12877-015-0166-1.
Daamen MA, Hamers JP, Gorgels AP, et al. 2016. Treatment of heart failure in nursing home residents. Journal of Geriatric Cardiology 13(1): 44–50. DOI: 10.11909/j.issn.1671-5411.2016.01.001.
Heckman GA, Boscart VM, Huson K, et al. 2018. Enhancing Knowledge and InterProfessional care for Heart Failure (EKWIP-HF) in long-term care: a pilot study. Pilot and Feasibility Studies 4(9): 1–11. DOI: 10.1186/s40814-017-0153-8.
Kerr S, Penney L, Barnes HM, et al. 2010. Kaupapa Maori action research to improve heart disease services in Aotearoa, New Zealand. Ethnicity and Health 15(1). DOI: 10.1080/13557850903374476.
Mebazaa A, Yilmaz MB, Levy P, et al. 2015. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. European Journal of Heart Failure 17(6): 544–58. DOI: 10.1002/ejhf.289.
Miner-Williams W. 2017. Racial inequities in cardiovascular disease in New Zealand. Diversity and Equality in Health and Care 14(1): 23–33. URL: diversityhealthcare.imedpub.com/racial-inequities-in-cardiovascular-disease-in-newzealand.pdf.
Ministry of Health. 2018. Cardiovascular disease. URL: www.health.govt.nz/our-work/populations/maori-health/tatau-kahukura-maori-health-statistics/nga-mana-hauora-tutohu-health-status-indicators/cardiovascular-disease.
Riley J. 2015. The key roles for the nurse in acute heart failure management. Cardiac Failure Review 1(2): 123–7. DOI: 10.15420/cfr.2015.1.2.123.
Selak V, Poppe K, Grey C, et al. 2020. Ethnic differences in cardiovascular risk profiles among 475,241 adults in primary care in Aotearoa, New Zealand. New Zealand Medical Journal 133(1521): 14–27. URL: pubmed.ncbi.nlm.nih.gov/32994634/.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
