| Single map | Consumer summary (156KB, PDF) |
This Atlas of Healthcare Variation domain gives rates for children aged 0–14 having surgery for:
- tonsillectomy (removal of one or both tonsils)
- ventilation tube (grommet) insertion.
The data was taken from the National Minimum Dataset. It presents rates of publicly funded procedures by district health board (DHB), over a 10-year period (2009–18), by age group, gender and ethnic group. Available data was not sufficiently robust to allow analysis of the indications for surgery.
As before, this Atlas domain does not include privately funded surgeries. If data from private hospitals was included, the procedure rates are likely to change most in the larger cities.
Where there is significant variation in rates, we can ask: is this variation is warranted and based on genuine differences between populations or are other factors at play?
The ideal surgery rate for both procedures is not known.
Surgical procedures
Updated September 2020 (data up to 2018)
Tonsillectomy
- From 2009 to 2018, tonsillectomy rates remained steady at around 3.6–4.0 per 1,000 children.
- Tonsillectomy rates were significantly higher in non-Māori, non-Pacific children compared with Māori and Pacific children.
- The level of variation between DHBs remained around three-fold.
Grommet insertion
- The significant reduction in average grommet insertion rates since 2013 was sustained through 2018.
- The level of variation between DHBs remained greater than two-fold.
- Rates were highest in European/other children aged 0–4 years despite evidence suggesting Māori and Pacific children aged 0–9 years have the highest prevalence of otitis media (middle ear infection)[1, 2].

Tonsillectomy rates have remained steady over the last six years; rates were significantly higher for non-Māori, non-Pacific children.
- From 2009 to 2018 the average tonsillectomy rate in Aotearoa New Zealand remained fairly steady at around 3.6–4.0 per 1,000 children.
- There was a significant difference between ethnic groups: Asian peoples had the lowest tonsillectomy rates whereas European/other had the highest.
- As expected, rates were significantly lower in children aged 10–14 years compared with those aged 5–9 years.
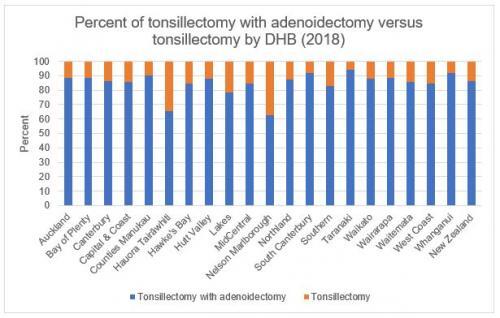
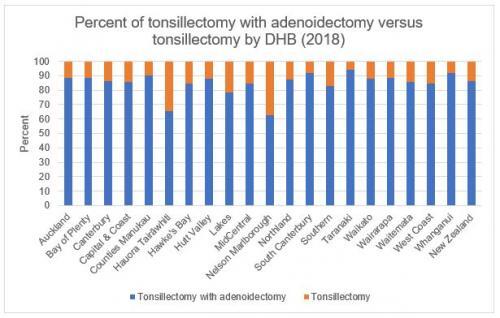
- Eighty-six percent of operations were tonsillectomy with adenoidectomy (removal of adenoids) with 14 percent tonsillectomy alone.
- Around one-third of operations had a diagnosis code of obstructive sleep apnoea (any diagnosis).
Grommet insertion rates were lower than in 2009–13
- From 2009 to 2018 there was a significant reduction in the average grommet insertion rate from 7.2 per 1,000 children in 2009 to 5.3 per 1,000 children in 2018.
- Grommet insertion rates were highest in European/other children aged 0–4 years despite evidence suggesting Māori and Pacific children aged 0–9 years have the highest prevalence of otitis media [1, 2].
Table 1: Ventilation tube insertion rates per 1,000 by age and ethnicity (2018)
95 percent confidence intervals are shown in brackets. Italics is used to indicate where rates are significantly higher.
| Ethnicity | Age groups (years) | |||
| 0–4 | 5–9 | 10–14 | Total | |
| Māori |
9.9 (9.2–10.5) |
7.1 (6.5–7.6) |
2.1 (1.8–2.4) |
6.4 (6.1–6.7) |
| Pacific peoples |
7.8 (6.8–8.9) |
7.0 (6.1–8.0) |
2.8 (2.2–3.4) |
5.9 (5.4–6.4) |
| Asian |
3.6 (3.1–4.1) |
2.2 (1.8–2.6) |
0.3 (0.1–0.5) |
2.2 (1.9–2.4) |
| European/other |
11.3 (10.7–11.9) |
5.2 (4.8–5.5) |
1.0 (0.8–1.2) |
5.6 (5.3–5.8) |
| Total |
9.3 (8.9–9.6) |
5.4 (5.2–5.7) |
1.4 (1.2–1.5) |
5.3 (5.2–5.5) |
Otitis media rates are believed to be higher in Māori and Pacific children although accurate estimates of national rates in primary care are not available. Data from 2002–08 shows that acute hospitalisations for otitis media were significantly higher in Māori and Pacific children than in European/other children, both at ages 0–4 and 5–9 years [1]. The Deafness Notification Database reports that Māori children are more likely to have a hearing loss than European/other children [2]. This report found Māori children have both higher rates of mild and moderate hearing loss and higher rates of bilateral loss (hearing loss in both ears) [2]. Report data also suggested that Pacific children may have higher rates of bilateral hearing loss than European/other.
The grommet insertion rate for European/other children halved from ages 0–4 to 5–9 years but not in Māori or Pacific children. It may be that routine before school check hearing screening is identifying the need for intervention in school-age Māori and Pacific children [1]. A study of asymptomatic preschool (three-year-old) children in South Auckland found 22 percent had unsuspected ear disease and hearing loss [3]. Māori and Pacific children were more likely to have hearing loss. This may mean grommet insertion rates are not matching population need.
Tonsillectomy
Tonsillectomy is the removal of one or both tonsils, usually in response to repeat acute tonsillitis or to treat sleep-disordered breathing. Usually the adenoids are removed at the same time – this is known as an adenotonsillectomy.
For the treatment of repeat acute tonsillitis, the criteria for surgery are based on the number of episodes in a six- or 12-month period; typically this is around six or more clinically significant sore-throat episodes in one year, or fewer attacks occurring annually over two or more years. Recent international guidance recommends watchful waiting for people with mild sore throats and recommends that surgery only be performed when the sore throat is disabling and prevents normal functioning [4].
Sleep-disordered breathing and obstructive sleep apnoea are conditions where the upper airway obstruction during sleep results in poor-quality sleep, daytime fatigue, poor school performance and, in severe cases, serious disorders of cardiopulmonary (heart and lung) function.
Grommet insertion
Otitis media (middle ear infection) is a common childhood infection, with up to 80 percent of children estimated to have at least one episode by three years of age [5].
Otitis media is most commonly caused by Eustachian tube dysfunction as a result of swollen mucous membranes in the nasopharynx (the upper part of the throat behind the nose), itself a result of upper respiratory tract infection or allergy. There are three types of otitis media:
- acute otitis media
- recurrent acute otitis media
- otitis media with effusion.
In Aotearoa New Zealand, acute otitis media (AOM) has been estimated to affect 273 per 1,000 children aged 0–4 years every year [6]. Of these, 74 percent of children have one episode, while 4 percent may experience recurrent AOM. Recurrent AOM is characterised by repeat acute middle ear infections, typically defined as to three to six infections over six months or six or more episodes in a year.
Otitis media with effusion (OME, or ‘glue ear’) is the presence of fluid (effusion) in the middle ear without an acute infection. OME is common, with two peaks in young children at two and five years of age. By 10 years of age, 80 percent of children will have had at least one episode [7] and most episodes resolve by themselves.
Children who have recurrent AOM or OME may need surgery to insert grommets. The decision to operate is usually based on two factors:
- the number of episodes of AOM experienced over six months or a year, and/or
- the presence of symptoms such as hearing loss, speech and language delay, and learning problems associated with a middle ear effusion affecting both ears and documented as present for three months or longer.
Systematic reviews report that grommet insertion improves hearing for those with OME and associated hearing loss during the first six months of follow-up but that there is no effect on language development or cognition in otherwise healthy children [7, 8]. For children with recurrent AOM, systematic reviews indicate grommets help to prevent/reduce infections in the first six months [9]. Most grommets last between six and 12 months. Evidence suggests that parents notice improvement in general health, behaviour and social skills in their children after grommet insertion, however, the quality of the studies does not allow strong conclusions to be drawn.
The Atlas presents data in the context of Aotearoa New Zealand only. Here, rates of both recurrent AOM and OME are higher in Māori and Pacific populations. As these populations are not represented in international studies, international guidelines should be interpreted with some caution.
Questions the data might prompt:
- Do DHBs have referral and intervention guidelines that are based on international best practice and agreed between general practitioners and surgeons?
- For each procedure, what are the most common indications for surgery?
- How do factors such as resource allocation or the availability of private surgery influence intervention rates?
- Does the uptake of private health insurance impact on the number of tonsillectomy and grommet insertion operations done in public hospitals? Are rates of private insurance uptake changing?
- Is the observed variation clinically meaningful?
- Should intervention rates be higher in Pacific and Māori children?
- Do DHBs with low grommet insertion rates have higher rates of tympanoplasty (operation to reconstruct the eardrum) and mastoidectomy (operation to remove mastoid air cells), reflecting higher rates of untreated middle ear disease?
- Do high rates for grommet insertion lead to high later myringoplasty rates, reflecting persistent tympanic membrane perforation (ruptured eardrum) after grommet extrusion (typically grommets fall out on their own)?
- Byars SG, Stearns SC, Boomsma JJ. 2018. Association of Long-Term Risk of Respiratory, Allergic, and Infectious Diseases With Removal of Adenoids and Tonsils in Childhood. JAMA Otolaryngol Head Neck Surg. DOI: 10.1001/jamaoto.2018.0614. URL: https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2683621 (accessed June 2018).
- BPAC. 2012. Otitis media: a common childhood illness. Best Practice Journal 46. URL: https://bpac.org.nz/bpj/2012/september/otitismedia.aspx.
- McCallum J, Craig L, Whittaker I, et al. 2015. Ethnic differences in acute hospitalisations for otitis media and elective hospitalisations for ventilation tubes in New Zealand children aged 0–14 years. NZMJ 128(1416): 10–20.
- Digby JE, Purdy SC, Kelly AS. 2018. Deafness Notification Report (2017) Hearing loss (not remediable by grommets) in New Zealanders under the age of 19. Auckland: Enable New Zealand.
- Dickinson LJ, Nimmo M, Morton RP, et al. 2018. 'Asymptomatic' South Auckland preschool children have significant hearing loss and middle ear disease. Int J Pediatr Otorhinolaryngol 114: 106‒10.
- SIGN. 2010. Management of sore throat and indications for tonsillectomy, in SIGN sore throat guideline 2010. URL: https://www.sign.ac.uk/our-guidelines/management-of-sore-throat-and-indications-for-tonsillectomy/.
- Teele DW, Klein JO, Rosner B. 1989. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis 160(1): 83–94.
- Gribben B, Salkeld LJ, Hoare S, et al. 2012. The incidence of acute otitis media in New Zealand children under five years of age in the primary care setting. J Prim Health Care 4(3): 205–12.
- National Collaborating Centre for Women’s and Children’s Health. 2008. Surgical management of otitis media with effusion in children. Commissioned by the National Institute for Health and Clinical Excellence.
- Browning GG, Rovers MM, Williamson I, et al. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev 2010, Issue 10, Art. No. CD001801.
- McDonald S, Langton Hewer CD, Nunez DA. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database Syst Rev 2008, Issue 4, Art. No. CD004741.
Domain update
Updated September 2020 (data up to 2018)
Tonsillectomy
- From 2009 to 2018, tonsillectomy rates remained steady at around 3.6–4.0 per 1,000 children.
- Tonsillectomy rates were significantly higher in non-Māori, non-Pacific children compared with Māori and Pacific children.
- The level of variation between DHBs remained around three-fold.
Grommet insertion
- The significant reduction in average grommet insertion rates since 2013 was sustained through 2018.
- The level of variation between DHBs remained greater than two-fold.
- Rates were highest in European/other children aged 0–4 years despite evidence suggesting Māori and Pacific children aged 0–9 years have the highest prevalence of otitis media (middle ear infection)[1, 2].

Tonsillectomy rates have remained steady over the last six years; rates were significantly higher for non-Māori, non-Pacific children.
- From 2009 to 2018 the average tonsillectomy rate in Aotearoa New Zealand remained fairly steady at around 3.6–4.0 per 1,000 children.
- There was a significant difference between ethnic groups: Asian peoples had the lowest tonsillectomy rates whereas European/other had the highest.
- As expected, rates were significantly lower in children aged 10–14 years compared with those aged 5–9 years.
- Eighty-six percent of operations were tonsillectomy with adenoidectomy (removal of adenoids) with 14 percent tonsillectomy alone.
- Around one-third of operations had a diagnosis code of obstructive sleep apnoea (any diagnosis).
Grommet insertion rates were lower than in 2009–13
- From 2009 to 2018 there was a significant reduction in the average grommet insertion rate from 7.2 per 1,000 children in 2009 to 5.3 per 1,000 children in 2018.
- Grommet insertion rates were highest in European/other children aged 0–4 years despite evidence suggesting Māori and Pacific children aged 0–9 years have the highest prevalence of otitis media [1, 2].
Table 1: Ventilation tube insertion rates per 1,000 by age and ethnicity (2018)
95 percent confidence intervals are shown in brackets. Italics is used to indicate where rates are significantly higher.
| Ethnicity | Age groups (years) | |||
| 0–4 | 5–9 | 10–14 | Total | |
| Māori |
9.9 (9.2–10.5) |
7.1 (6.5–7.6) |
2.1 (1.8–2.4) |
6.4 (6.1–6.7) |
| Pacific peoples |
7.8 (6.8–8.9) |
7.0 (6.1–8.0) |
2.8 (2.2–3.4) |
5.9 (5.4–6.4) |
| Asian |
3.6 (3.1–4.1) |
2.2 (1.8–2.6) |
0.3 (0.1–0.5) |
2.2 (1.9–2.4) |
| European/other |
11.3 (10.7–11.9) |
5.2 (4.8–5.5) |
1.0 (0.8–1.2) |
5.6 (5.3–5.8) |
| Total |
9.3 (8.9–9.6) |
5.4 (5.2–5.7) |
1.4 (1.2–1.5) |
5.3 (5.2–5.5) |
Otitis media rates are believed to be higher in Māori and Pacific children although accurate estimates of national rates in primary care are not available. Data from 2002–08 shows that acute hospitalisations for otitis media were significantly higher in Māori and Pacific children than in European/other children, both at ages 0–4 and 5–9 years [1]. The Deafness Notification Database reports that Māori children are more likely to have a hearing loss than European/other children [2]. This report found Māori children have both higher rates of mild and moderate hearing loss and higher rates of bilateral loss (hearing loss in both ears) [2]. Report data also suggested that Pacific children may have higher rates of bilateral hearing loss than European/other.
The grommet insertion rate for European/other children halved from ages 0–4 to 5–9 years but not in Māori or Pacific children. It may be that routine before school check hearing screening is identifying the need for intervention in school-age Māori and Pacific children [1]. A study of asymptomatic preschool (three-year-old) children in South Auckland found 22 percent had unsuspected ear disease and hearing loss [3]. Māori and Pacific children were more likely to have hearing loss. This may mean grommet insertion rates are not matching population need.
About the two procedures
Tonsillectomy
Tonsillectomy is the removal of one or both tonsils, usually in response to repeat acute tonsillitis or to treat sleep-disordered breathing. Usually the adenoids are removed at the same time – this is known as an adenotonsillectomy.
For the treatment of repeat acute tonsillitis, the criteria for surgery are based on the number of episodes in a six- or 12-month period; typically this is around six or more clinically significant sore-throat episodes in one year, or fewer attacks occurring annually over two or more years. Recent international guidance recommends watchful waiting for people with mild sore throats and recommends that surgery only be performed when the sore throat is disabling and prevents normal functioning [4].
Sleep-disordered breathing and obstructive sleep apnoea are conditions where the upper airway obstruction during sleep results in poor-quality sleep, daytime fatigue, poor school performance and, in severe cases, serious disorders of cardiopulmonary (heart and lung) function.
Grommet insertion
Otitis media (middle ear infection) is a common childhood infection, with up to 80 percent of children estimated to have at least one episode by three years of age [5].
Otitis media is most commonly caused by Eustachian tube dysfunction as a result of swollen mucous membranes in the nasopharynx (the upper part of the throat behind the nose), itself a result of upper respiratory tract infection or allergy. There are three types of otitis media:
- acute otitis media
- recurrent acute otitis media
- otitis media with effusion.
In Aotearoa New Zealand, acute otitis media (AOM) has been estimated to affect 273 per 1,000 children aged 0–4 years every year [6]. Of these, 74 percent of children have one episode, while 4 percent may experience recurrent AOM. Recurrent AOM is characterised by repeat acute middle ear infections, typically defined as to three to six infections over six months or six or more episodes in a year.
Otitis media with effusion (OME, or ‘glue ear’) is the presence of fluid (effusion) in the middle ear without an acute infection. OME is common, with two peaks in young children at two and five years of age. By 10 years of age, 80 percent of children will have had at least one episode [7] and most episodes resolve by themselves.
Children who have recurrent AOM or OME may need surgery to insert grommets. The decision to operate is usually based on two factors:
- the number of episodes of AOM experienced over six months or a year, and/or
- the presence of symptoms such as hearing loss, speech and language delay, and learning problems associated with a middle ear effusion affecting both ears and documented as present for three months or longer.
Systematic reviews report that grommet insertion improves hearing for those with OME and associated hearing loss during the first six months of follow-up but that there is no effect on language development or cognition in otherwise healthy children [7, 8]. For children with recurrent AOM, systematic reviews indicate grommets help to prevent/reduce infections in the first six months [9]. Most grommets last between six and 12 months. Evidence suggests that parents notice improvement in general health, behaviour and social skills in their children after grommet insertion, however, the quality of the studies does not allow strong conclusions to be drawn.
The context of this data
The Atlas presents data in the context of Aotearoa New Zealand only. Here, rates of both recurrent AOM and OME are higher in Māori and Pacific populations. As these populations are not represented in international studies, international guidelines should be interpreted with some caution.
Questions the data might prompt:
- Do DHBs have referral and intervention guidelines that are based on international best practice and agreed between general practitioners and surgeons?
- For each procedure, what are the most common indications for surgery?
- How do factors such as resource allocation or the availability of private surgery influence intervention rates?
- Does the uptake of private health insurance impact on the number of tonsillectomy and grommet insertion operations done in public hospitals? Are rates of private insurance uptake changing?
- Is the observed variation clinically meaningful?
- Should intervention rates be higher in Pacific and Māori children?
- Do DHBs with low grommet insertion rates have higher rates of tympanoplasty (operation to reconstruct the eardrum) and mastoidectomy (operation to remove mastoid air cells), reflecting higher rates of untreated middle ear disease?
- Do high rates for grommet insertion lead to high later myringoplasty rates, reflecting persistent tympanic membrane perforation (ruptured eardrum) after grommet extrusion (typically grommets fall out on their own)?
Reading list
- Byars SG, Stearns SC, Boomsma JJ. 2018. Association of Long-Term Risk of Respiratory, Allergic, and Infectious Diseases With Removal of Adenoids and Tonsils in Childhood. JAMA Otolaryngol Head Neck Surg. DOI: 10.1001/jamaoto.2018.0614. URL: https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2683621 (accessed June 2018).
- BPAC. 2012. Otitis media: a common childhood illness. Best Practice Journal 46. URL: https://bpac.org.nz/bpj/2012/september/otitismedia.aspx.
References
- McCallum J, Craig L, Whittaker I, et al. 2015. Ethnic differences in acute hospitalisations for otitis media and elective hospitalisations for ventilation tubes in New Zealand children aged 0–14 years. NZMJ 128(1416): 10–20.
- Digby JE, Purdy SC, Kelly AS. 2018. Deafness Notification Report (2017) Hearing loss (not remediable by grommets) in New Zealanders under the age of 19. Auckland: Enable New Zealand.
- Dickinson LJ, Nimmo M, Morton RP, et al. 2018. 'Asymptomatic' South Auckland preschool children have significant hearing loss and middle ear disease. Int J Pediatr Otorhinolaryngol 114: 106‒10.
- SIGN. 2010. Management of sore throat and indications for tonsillectomy, in SIGN sore throat guideline 2010. URL: https://www.sign.ac.uk/our-guidelines/management-of-sore-throat-and-indications-for-tonsillectomy/.
- Teele DW, Klein JO, Rosner B. 1989. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis 160(1): 83–94.
- Gribben B, Salkeld LJ, Hoare S, et al. 2012. The incidence of acute otitis media in New Zealand children under five years of age in the primary care setting. J Prim Health Care 4(3): 205–12.
- National Collaborating Centre for Women’s and Children’s Health. 2008. Surgical management of otitis media with effusion in children. Commissioned by the National Institute for Health and Clinical Excellence.
- Browning GG, Rovers MM, Williamson I, et al. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev 2010, Issue 10, Art. No. CD001801.
- McDonald S, Langton Hewer CD, Nunez DA. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database Syst Rev 2008, Issue 4, Art. No. CD004741.
