Health service access
This Atlas domain uses information reported by patients about their experience with health services and builds on what we already know from the New Zealand primary care patient experience surveys for 2018 and 2019. It reports on responses to seven questions across two survey years to investigate whether there are differences by geographic region and/or patient demographic. These questions were selected as being key for understanding patient’s experience of accessing and using health services.
Access to health care is distinct from utilisation of health care.[1] There is a growing body of evidence describing poorer access among socially disadvantaged groups in Aotearoa New Zealand[2, 3] including our report A window on the quality of Aotearoa New Zealand’s health care 2019 – a view on Māori health equity.
While a different number of people responded to each survey question, on average over 79,000 people answered each of the questions reported here; of these, around 6,500 were Māori, 1,900 Pacific peoples, 3,900 Asian and 67,000 Other ethnic group.
In this domain, we present unweighted responses and weighted scores. The weighted scores use the population structure who attended primary care in each district health board (DHB) (ie, those potentially eligible to participate) (age, gender and ethnicity) and compares this with the respondent structure (ie, the age, gender and ethnicity of those who responded to the survey). This creates a co-efficient, which is applied to the results of the survey. This then increases or decreases a particular score and provides a weighted result. For further information, including number of responses by age and ethnicity, please view the methodology (278KB, pdf).
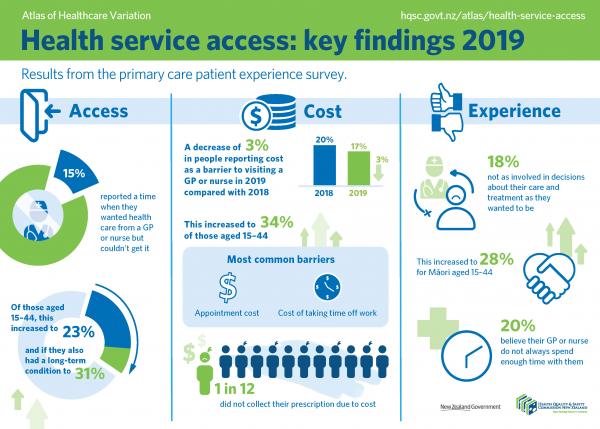
An infographic summarising the key findings is shown below and can be downloaded as a PDF here (1.63MB, pdf).
Updated 2020
Key messages
- There was a decrease of 3 percent of people who reported cost as a barrier to visiting a GP or nurse in 2019 compared with 2018, from 20 percent to 17 percent of respondents. This statistically significant decrease is consistent with the decrease of 1.5 percent in the New Zealand Health Survey (NZHS 18/19) question, ‘In the past 12 months, was there a time when you had a medical problem but did not visit a GP because of cost?’. This decrease is seen across all age groups, genders and ethnic groups.
- Eight percent of respondents reported that cost stopped them from picking up a prescription in 2019, down from 9 percent in 2018. This decrease was statistically significant.
Note: all the differences between age, gender and ethnicity noted in the text below are statistically significant.
Question: Was there ever a time when you wanted health care from a GP or nurse but you couldn't get it?
One in seven respondents (15 percent) reported a time when they wanted health care from a GP or nurse but couldn't get it.
- Women were more likely (18 percent) than men (11 percent) to report this/a time when they wanted health care from a GP or nurse but couldn’t get it. There was a clear age gradient, with 23 percent of those aged 15–44 years unable to get care compared with less than 10 percent of those aged 65 years and over.
- Twenty-four percent of Māori aged 15–64 years reported being unable to get care compared with 19 percent of Asian and Other.
- People reporting a long-term condition were more likely to report being unable to get care than those without a long-term condition, at all ages. For example, of 15–24-year-olds, 30 percent with a long-term condition reported this compared with 20 percent with no long-term condition. For all age groups, the rate was higher for those with self-reported arthritis or long-term pain, asthma or chronic obstructive pulmonary disease or a mental health condition.
- The percentage of people who reported being unable to get care varied widely between DHBs, from 8 percent to 27 percent of respondents.
- This question comes after people have already identified cost as possible barrier. Respondents’ answers often relate to appointment availability, particularly to see their usual doctor at short notice; the wait time for the appointment once they reached the clinic; and clinic hours not being compatible with work hours – a particular issue when patients wanted care urgently.
Question: In the last 12 months was there a time when you did not visit a GP or nurse because of cost?
One in six respondents (17 percent) reported not visiting a GP or nurse because of cost in the last 12 months.
- There was a decrease of 3 percent of people who reported cost as a barrier in 2019, compared with 2018, from 20 percent to 17 percent of respondents. This decrease is consistent with the decrease of 1.5 percent in the NZHS 18/19 question, ‘In the past 12 months, was there a time when you had a medical problem but did not visit a GP because of cost?’. The NZHS surveys a random sample of people from the population whereas this survey focuses on people who have accessed a primary care service.
- This increased to 43 percent of those aged 15–24 years with any long-term condition.
- Twenty percent of women and 11 percent of men reported not visiting their GP or nurse in the previous year due to cost.
- Younger people reported cost as a barrier to a far greater extent than older people: 34 percent of those aged 15–44 years compared with 8 percent of people aged 65 years and over.
- Age–sex stratified analyses show 39 percent of 15–24-year-old females reported not visiting their GP or nurse at some point in the year due to cost compared with 26 percent of males in the same age group.
- The percentage of people reporting cost as a barrier varied between DHBs, from 8 percent to 22 percent of respondents.
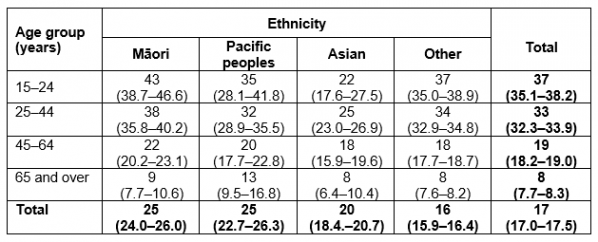
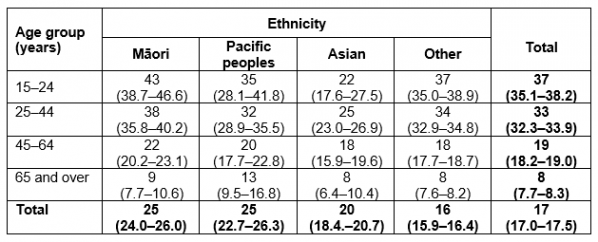
Percentage of people who report not visiting a GP or nurse due to cost in the last 12 months (2019). Confidence intervals calculated at 95 percent are shown in brackets.
Question: Could you tell us why cost stopped you from seeing a GP or nurse?
Appointment cost was the most common cost barrier.
- Of the 8 percent aged 65 years and over for whom cost was a barrier, appointment cost was the barrier for 95 percent of those respondents. In comparison, appointment cost was a barrier for 89 percent of those aged under 65 years.
- Twenty-nine percent of those aged under 65 years reported the cost of taking time off work prevented them from accessing care. As might be expected, 5 percent of those aged 65 years and over reported this as an issue.
- Transport cost was a significantly greater barrier for Māori and Pacific peoples, at 19 percent compared with around 8 percent for Asian and Other ethnic groups.
Question: Has cost stopped you from picking up a prescription?
Eight percent of respondents reported that cost had stopped them from picking up a prescription.
- One percent fewer respondents reported cost stopped them from picking up a prescription compared with the previous year. This decrease is consistent with the decrease of 1.3 percent in the NZHS (18/19) question, ‘In the past 12 months, was there a time when you got a prescription for yourself but did not collect one or more prescription items from the pharmacy or chemist because of cost? (Yes, no, don’t know, refused)’. The NZHS surveys a random sample of people from the population whereas this survey focuses on people who have accessed a primary care service.
- There was a clear age effect, with 19 percent of 15–24-year-olds reporting this barrier compared with 1 percent of those aged 75 years and over.
- At all ages, people who reported a long-term condition were more likely to report not collecting a prescription due to cost than people reporting no long-term conditions, although the difference was most pronounced in those aged under 65 years.
- Women were much more likely than men to report not collecting a prescription due to cost – 9 percent compared with 5 percent.
- People of Māori and Pacific ethnicity reported prescription cost as a barrier more than Asian and Other populations.
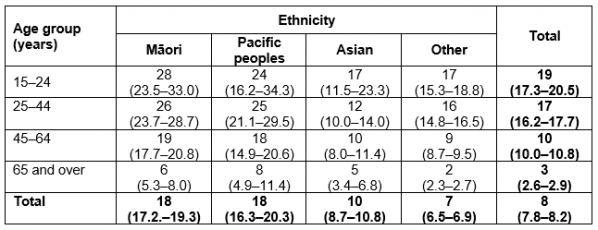
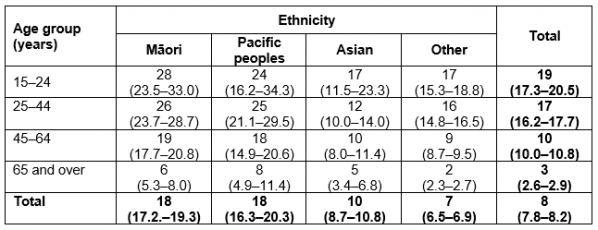
Percentage of people reporting not picking up a medicine due to cost in the past year by age and ethnicity (2019). Confidence intervals calculated at 95 percent are shown in brackets.
Question: have you been involved in decisions about your care and treatment as much as you wanted to be?
Overall, 18 percent of people were not as involved in decisions about their care and treatment as they wanted to be.
- Nineteen percent of women and 16 percent of men reported not being as involved in decisions about their care and treatment as much as they wanted to be.
- While around 2 percent of people were not as involved as much as they wanted to be, 16 percent of people were only involved as much as they wanted to be to some extent.
- Younger people reported less involvement, with 30 percent of 15–24-year-olds being involved either to some extent or not at all, compared with 14 percent of those aged 65 years and over.
- The percentage of people not as involved as much as they wanted to be varied more than two-fold between DHBs, from 14 percent to 31 percent of respondents.
Question: does your GP or nurse spend enough time with you?
Twenty percent of patients did not agree that their GP or nurse always spent enough time with them.
- Younger people were less likely to report enough time being spent with them, with 33 percent of 15–24-year olds answering ‘yes, sometimes’ or ‘no’ compared with 15 percent of those aged 65 years and over.
- There were limited differences by ethnicity.
- The percentage of people reporting that their GP or nurse did not always spend enough time with them varied two-fold between DHBs, from 16 percent to 32 percent of respondents.
Question: You said you did not always follow the instructions when you took the medication. Please tell us why.
Eight percent of respondents said they did not always follow the instructions when they took medication.
- This ranged from 17 percent of 15–24-year-olds to 5 percent of those aged 65 years and over.
- This question highlights that patients are not always sufficiently informed and engaged to take medicines as prescribed.
- When asked the reason why, 68 percent of people said they forgot and 25 percent said they experienced side effects. Younger people were more likely to report forgetting to take their medicine while older people were more likely to report experiencing side effects.
Background
This Atlas domain uses information reported by patients about their experience with health services and builds on what we already know from the New Zealand primary care patient experience surveys for 2018 and 2019. It reports on responses to seven questions across two survey years to investigate whether there are differences by geographic region and/or patient demographic. These questions were selected as being key for understanding patient’s experience of accessing and using health services.
Access to health care is distinct from utilisation of health care.[1] There is a growing body of evidence describing poorer access among socially disadvantaged groups in Aotearoa New Zealand[2, 3] including our report A window on the quality of Aotearoa New Zealand’s health care 2019 – a view on Māori health equity.
While a different number of people responded to each survey question, on average over 79,000 people answered each of the questions reported here; of these, around 6,500 were Māori, 1,900 Pacific peoples, 3,900 Asian and 67,000 Other ethnic group.
In this domain, we present unweighted responses and weighted scores. The weighted scores use the population structure who attended primary care in each district health board (DHB) (ie, those potentially eligible to participate) (age, gender and ethnicity) and compares this with the respondent structure (ie, the age, gender and ethnicity of those who responded to the survey). This creates a co-efficient, which is applied to the results of the survey. This then increases or decreases a particular score and provides a weighted result. For further information, including number of responses by age and ethnicity, please view the methodology (278KB, pdf).
Key findings summary
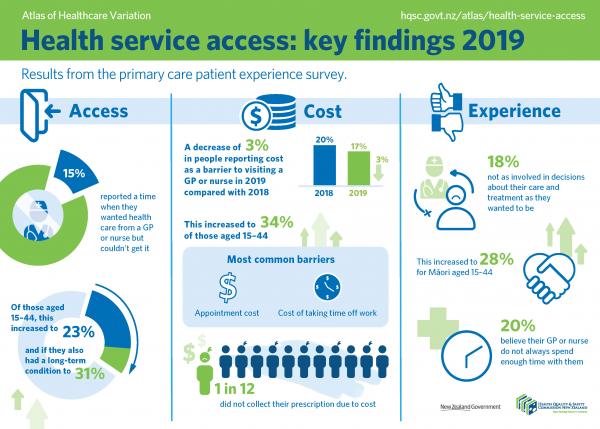
An infographic summarising the key findings is shown below and can be downloaded as a PDF here (1.63MB, pdf).
Updated 2020
Key messages
- There was a decrease of 3 percent of people who reported cost as a barrier to visiting a GP or nurse in 2019 compared with 2018, from 20 percent to 17 percent of respondents. This statistically significant decrease is consistent with the decrease of 1.5 percent in the New Zealand Health Survey (NZHS 18/19) question, ‘In the past 12 months, was there a time when you had a medical problem but did not visit a GP because of cost?’. This decrease is seen across all age groups, genders and ethnic groups.
- Eight percent of respondents reported that cost stopped them from picking up a prescription in 2019, down from 9 percent in 2018. This decrease was statistically significant.
Key findings by question
Note: all the differences between age, gender and ethnicity noted in the text below are statistically significant.
Question: Was there ever a time when you wanted health care from a GP or nurse but you couldn't get it?
One in seven respondents (15 percent) reported a time when they wanted health care from a GP or nurse but couldn't get it.
- Women were more likely (18 percent) than men (11 percent) to report this/a time when they wanted health care from a GP or nurse but couldn’t get it. There was a clear age gradient, with 23 percent of those aged 15–44 years unable to get care compared with less than 10 percent of those aged 65 years and over.
- Twenty-four percent of Māori aged 15–64 years reported being unable to get care compared with 19 percent of Asian and Other.
- People reporting a long-term condition were more likely to report being unable to get care than those without a long-term condition, at all ages. For example, of 15–24-year-olds, 30 percent with a long-term condition reported this compared with 20 percent with no long-term condition. For all age groups, the rate was higher for those with self-reported arthritis or long-term pain, asthma or chronic obstructive pulmonary disease or a mental health condition.
- The percentage of people who reported being unable to get care varied widely between DHBs, from 8 percent to 27 percent of respondents.
- This question comes after people have already identified cost as possible barrier. Respondents’ answers often relate to appointment availability, particularly to see their usual doctor at short notice; the wait time for the appointment once they reached the clinic; and clinic hours not being compatible with work hours – a particular issue when patients wanted care urgently.
Question: In the last 12 months was there a time when you did not visit a GP or nurse because of cost?
One in six respondents (17 percent) reported not visiting a GP or nurse because of cost in the last 12 months.
- There was a decrease of 3 percent of people who reported cost as a barrier in 2019, compared with 2018, from 20 percent to 17 percent of respondents. This decrease is consistent with the decrease of 1.5 percent in the NZHS 18/19 question, ‘In the past 12 months, was there a time when you had a medical problem but did not visit a GP because of cost?’. The NZHS surveys a random sample of people from the population whereas this survey focuses on people who have accessed a primary care service.
- This increased to 43 percent of those aged 15–24 years with any long-term condition.
- Twenty percent of women and 11 percent of men reported not visiting their GP or nurse in the previous year due to cost.
- Younger people reported cost as a barrier to a far greater extent than older people: 34 percent of those aged 15–44 years compared with 8 percent of people aged 65 years and over.
- Age–sex stratified analyses show 39 percent of 15–24-year-old females reported not visiting their GP or nurse at some point in the year due to cost compared with 26 percent of males in the same age group.
- The percentage of people reporting cost as a barrier varied between DHBs, from 8 percent to 22 percent of respondents.
Percentage of people who report not visiting a GP or nurse due to cost in the last 12 months (2019). Confidence intervals calculated at 95 percent are shown in brackets.
Question: Could you tell us why cost stopped you from seeing a GP or nurse?
Appointment cost was the most common cost barrier.
- Of the 8 percent aged 65 years and over for whom cost was a barrier, appointment cost was the barrier for 95 percent of those respondents. In comparison, appointment cost was a barrier for 89 percent of those aged under 65 years.
- Twenty-nine percent of those aged under 65 years reported the cost of taking time off work prevented them from accessing care. As might be expected, 5 percent of those aged 65 years and over reported this as an issue.
- Transport cost was a significantly greater barrier for Māori and Pacific peoples, at 19 percent compared with around 8 percent for Asian and Other ethnic groups.
Question: Has cost stopped you from picking up a prescription?
Eight percent of respondents reported that cost had stopped them from picking up a prescription.
- One percent fewer respondents reported cost stopped them from picking up a prescription compared with the previous year. This decrease is consistent with the decrease of 1.3 percent in the NZHS (18/19) question, ‘In the past 12 months, was there a time when you got a prescription for yourself but did not collect one or more prescription items from the pharmacy or chemist because of cost? (Yes, no, don’t know, refused)’. The NZHS surveys a random sample of people from the population whereas this survey focuses on people who have accessed a primary care service.
- There was a clear age effect, with 19 percent of 15–24-year-olds reporting this barrier compared with 1 percent of those aged 75 years and over.
- At all ages, people who reported a long-term condition were more likely to report not collecting a prescription due to cost than people reporting no long-term conditions, although the difference was most pronounced in those aged under 65 years.
- Women were much more likely than men to report not collecting a prescription due to cost – 9 percent compared with 5 percent.
- People of Māori and Pacific ethnicity reported prescription cost as a barrier more than Asian and Other populations.
Percentage of people reporting not picking up a medicine due to cost in the past year by age and ethnicity (2019). Confidence intervals calculated at 95 percent are shown in brackets.
Question: have you been involved in decisions about your care and treatment as much as you wanted to be?
Overall, 18 percent of people were not as involved in decisions about their care and treatment as they wanted to be.
- Nineteen percent of women and 16 percent of men reported not being as involved in decisions about their care and treatment as much as they wanted to be.
- While around 2 percent of people were not as involved as much as they wanted to be, 16 percent of people were only involved as much as they wanted to be to some extent.
- Younger people reported less involvement, with 30 percent of 15–24-year-olds being involved either to some extent or not at all, compared with 14 percent of those aged 65 years and over.
- The percentage of people not as involved as much as they wanted to be varied more than two-fold between DHBs, from 14 percent to 31 percent of respondents.
Question: does your GP or nurse spend enough time with you?
Twenty percent of patients did not agree that their GP or nurse always spent enough time with them.
- Younger people were less likely to report enough time being spent with them, with 33 percent of 15–24-year olds answering ‘yes, sometimes’ or ‘no’ compared with 15 percent of those aged 65 years and over.
- There were limited differences by ethnicity.
- The percentage of people reporting that their GP or nurse did not always spend enough time with them varied two-fold between DHBs, from 16 percent to 32 percent of respondents.
Question: You said you did not always follow the instructions when you took the medication. Please tell us why.
Eight percent of respondents said they did not always follow the instructions when they took medication.
- This ranged from 17 percent of 15–24-year-olds to 5 percent of those aged 65 years and over.
- This question highlights that patients are not always sufficiently informed and engaged to take medicines as prescribed.
- When asked the reason why, 68 percent of people said they forgot and 25 percent said they experienced side effects. Younger people were more likely to report forgetting to take their medicine while older people were more likely to report experiencing side effects.
Health service use and the primary care patient experience survey: Key questions to answer as a provider
District health boards, primary health organisations and general practices all have access to the primary care patient experience survey reporting portal, which reports their patients’ responses to the survey.
We invite providers to answer the following questions:
- Does your organisation actively track your patients’ responses to the survey questions?
- Do you know which of your patient groups are experiencing the most barriers?
- Do you have a plan to address these barriers?
Below are questions for providers prompted by the findings in this domain, with an indication of whether the questions should be asked at a national organisation, DHB/PHO or general practice level.
Key questions to answer as a provider
National:
- How does this finding correlate with studies such as the Piper project,[1] which identified people being diagnosed late with cancer in emergency departments?
- Are there models of care that might work better?
- What is the GP full-time equivalent (FTE) per capita by region? What other models of care, such as nurse practitioners or health improvement practitioners, could be used?
- Are there sufficient GPs to serve the population?
- What are the downstream impacts for young people who are also experiencing high housing costs and high education costs? What is the longer-term impact on the future?
DHB/PHO and general practice:
- A quarter of women aged 25–44 years report unmet need. Do you know how many women in this age group there are in your region or practice?
- Who is experiencing unmet need (and why) in your region or practice?
- How can you work with the consumer groups who report the largest unmet need to co-design a better system?
- Do you have a high proportion of young or working-age enrolees? If so, would offering extended hours, telehealth or a patient portal help?
- What alternatives to a physical appointment does your practice offer, for example, a patient portal? How many patients report being able to get a response on the same day to an important question?
- When is your third next available appointment?
- Once patients arrive for their appointment, how long do they wait in the clinic for it to start?
- Jackson C, Sharples K, Firth M, et al. 2015. The PIPER Project. An Internal Examination of Colorectal Cancer Management in New Zealand. Wellington: Health Research Council and Ministry of Health. URL: https://bit.ly/3cXXjbE (accessed June 2019).
National:
- Have funding changes had the desired effect? For example, have community service card changes reduced unmet need?
DHB/PHO:
- How are DHBs and PHOs working to deliver a model of care that can help people better afford primary care and prescriptions?
- Do your patients know about low-cost access practices and how to find them?
General practice:
- Do your patients know that a community services card reduces appointment cost? Can you provide information on how to apply for a card at your practice?
- Are there subsidises (national or regional) that your patients might be eligible for? How do you inform your patients about these?
All providers:
- What percent of people also can’t access tests that have a cost, for example, x-rays?
- What are the impacts for those who can’t afford their medicine or who delay collecting it?
- What are the impacts on you and your patients when medicines are delayed or not collected?
- Are your patients given information on how to access the prescription subsidy scheme?
National and DHB/PHO:
- Are the models of care provided for young people appropriate? What youth services are available in your region, eg, youth one-stop-shops, and do your patients know how to access these?
- What are the implications of these findings given young people also experience greater barriers to accessing care? Are diagnoses and treatments properly explained?
General practice:
- How do these findings correlate with communication skills of staff at the practice?
National, DHB/PHO and general practice:
- What support does your population need to enable them to take their medicine as prescribed?
- Have you used the Health Quality & Safety Commission’s health literacy resources?
Fifteen percent of people reported unmet need for health care
National:
- How does this finding correlate with studies such as the Piper project,[1] which identified people being diagnosed late with cancer in emergency departments?
- Are there models of care that might work better?
- What is the GP full-time equivalent (FTE) per capita by region? What other models of care, such as nurse practitioners or health improvement practitioners, could be used?
- Are there sufficient GPs to serve the population?
- What are the downstream impacts for young people who are also experiencing high housing costs and high education costs? What is the longer-term impact on the future?
DHB/PHO and general practice:
- A quarter of women aged 25–44 years report unmet need. Do you know how many women in this age group there are in your region or practice?
- Who is experiencing unmet need (and why) in your region or practice?
- How can you work with the consumer groups who report the largest unmet need to co-design a better system?
- Do you have a high proportion of young or working-age enrolees? If so, would offering extended hours, telehealth or a patient portal help?
- What alternatives to a physical appointment does your practice offer, for example, a patient portal? How many patients report being able to get a response on the same day to an important question?
- When is your third next available appointment?
- Once patients arrive for their appointment, how long do they wait in the clinic for it to start?
- Jackson C, Sharples K, Firth M, et al. 2015. The PIPER Project. An Internal Examination of Colorectal Cancer Management in New Zealand. Wellington: Health Research Council and Ministry of Health. URL: https://bit.ly/3cXXjbE (accessed June 2019).
Seventeen percent of people reported not visiting a GP or nurse due to cost in the last 12 months
National:
- Have funding changes had the desired effect? For example, have community service card changes reduced unmet need?
DHB/PHO:
- How are DHBs and PHOs working to deliver a model of care that can help people better afford primary care and prescriptions?
- Do your patients know about low-cost access practices and how to find them?
General practice:
- Do your patients know that a community services card reduces appointment cost? Can you provide information on how to apply for a card at your practice?
- Are there subsidises (national or regional) that your patients might be eligible for? How do you inform your patients about these?
Eight percent of people reported cost stopped them from picking up a prescription
All providers:
- What percent of people also can’t access tests that have a cost, for example, x-rays?
- What are the impacts for those who can’t afford their medicine or who delay collecting it?
- What are the impacts on you and your patients when medicines are delayed or not collected?
- Are your patients given information on how to access the prescription subsidy scheme?
Younger people are more likely than older people to report not being as involved in decisions about their care as much as they want to be and are less likely than older people to report their GP or nurse spends enough time with them
National and DHB/PHO:
- Are the models of care provided for young people appropriate? What youth services are available in your region, eg, youth one-stop-shops, and do your patients know how to access these?
- What are the implications of these findings given young people also experience greater barriers to accessing care? Are diagnoses and treatments properly explained?
General practice:
- How do these findings correlate with communication skills of staff at the practice?
Eight percent of people did not always follow instructions when they took medicine
National, DHB/PHO and general practice:
- What support does your population need to enable them to take their medicine as prescribed?
- Have you used the Health Quality & Safety Commission’s health literacy resources?
References
- Levesque JF, Harris M, Russell G. 2013. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 12: 18.
- Ministry of Health. (nd). Indicator: Excellent, very good or good self-rated health. URL: https://minhealthnz.shinyapps.io/nz-health-survey-2018-19-annual-data-explorer/_w_f901ef64/#!/home.
- Metcalfe S, Beyene K, Urlich J, et al. 2018. Te Wero tonu—the challenge continues: Māori access to medicines 2006/07–2012/13 update. NZMJ 131(1485).
Resources
- Let’s plan for better care, a health literacy initiative to help consumers prepare well for their visit to the GP or other primary care health professional. It encourages people to plan ahead for practice visits and to ask questions when there, so they fully understand their diagnosis and treatment. It also suggests questions they can ask pharmacy staff when they pick up their medicine. This resource is also available in Chinese, Hindi, Māori and Samoan.
- Three steps to meeting health literacy needs | Ngā toru hīkoi e mōhiotia ai te hauora
- Communicating so people will understand, a poster for health professionals, which provides simple techniques for talking with people about their health or medicines.
- Medication ‘one-steps’. These resources are intended to:
- check some aspect of the safety system for a high-risk medicine in any area of work, whether on a ward, across a whole hospital or other care setting
- stimulate discussion about the system and what changes could be made to reduce the risk of harm from those medicines.
- Communication strategies at GP level from IHI.
- Choosing Wisely – resources for patients and practitioners to help with decisions relating to medicines, such as understanding what happens if people don’t take the medicine.
