| Infection single map | Infection double map | Consumer summary (121 KB, PDF) |
Infection and antibiotic use following major surgery
Infection and antibiotic use following major surgery gives clinicians, patients and health care providers an overview of the following by district health board (DHB):
- infections after major surgery in a public hospital
- postoperative sepsis rates
- community use of antibiotics in the 30 days after surgery in a public hospital.
This domain was created to explore areas of wide variation between DHBs and identify possible areas for local quality improvement.
Healthcare associated infections (HAIs) are some of the most common adverse events in health care worldwide. Up to 10 percent of patients admitted to hospitals in the developed world acquire one or more infections.[1] HAIs include central line-associated bloodstream infections, catheter-associated urinary tract infections, surgical site infections and ventilator-associated pneumonia.
- Adherence to best infection prevention and control measures, such as choice of skin antisepsis agent, surgical antimicrobial prophylaxis and appropriate hair removal, are crucial to minimise the risk of surgical site infections.[2]
- Surgical antimicrobial prophylaxis should be administered for the shortest effective period to minimise adverse effects, the development of antimicrobial resistance and costs. In most situations, a single dose given 0–60 minutes before the surgical incision is all that is required. For some procedures, additional doses given for a maximum of 24 hours postoperatively may occur.
- It is not best practice for antibiotics to be administered routinely postoperatively – the UK National Institute for Health and Care Excellence (NICE) recommends antibiotics are used only in cases where infection is suspected.[3]
- The data suggest that, on average, 32 percent of people had antibiotics within 30 days of major surgery. This compares with an inpatient recorded rate of infection of 2.3 percent and postoperative sepsis of 1.1 percent.
- For people undergoing surgery, ask how to care for your wound after surgery, what signs of infection to look for, and when to seek help. If taking antibiotics ensure you know when and how to long to take them for. For more information click here.
Many HAIs can be prevented by adherence to best practice with well-established processes that minimise infection risk. However, not all HAIs are preventable or relate to the quality of care.
Other known risk factors for HAIs among hospital patients include prolonged hospital stay, prolonged and/or inappropriate use of antibiotics, immunosuppression and other severe underlying conditions.
This domain aligns with the work of the Accident Compensation Corporation and the Health Quality & Safety Commission’s infection prevention and control programme, which has a range of initiatives to reduce HAIs. These include improving hand hygiene, improvement related to peripheral lines, preventing central line-associated bacteraemia and reducing surgical site infections. All DHBs are involved in these initiatives.
Note: This domain reports the number of infection events, not the number of people, thus one person may be counted multiple times. For all indicators (apart from indicator 8), patients were assigned to the DHB that provided treatment (DHB of service), not the DHB where they live. The risk of infection varies depending on the type of surgery and complexity of the surgical procedure. This means that DHBs with hospitals providing tertiary and quaternary services might be expected to have higher rates of infection, reflecting the higher complexity of surgical procedures performed. As an example, cardiac surgery is only performed in five DHBs.
Rate of infection following major surgery in a public hospital by DHB of service
- Infection is the most common complication of surgery; this indicator looks at infection rates directly linked to the surgery.
- In 2017, there was an average of 231 infections per 10,000 surgical discharges. This has decreased from 276 in 2011.
- Infection rates appear highest in the 45–64 age band. Rates have decreased in every age band from 2011 to 2017 except for the 25–44 band.
- There was no significant difference in infection rate between women and men.
- Māori had significantly higher rates than non-Māori, especially for women and 45–64-year-olds.
- There was limited DHB variation.
The total number of infections for men has reduced from around 700 in 2011 to around 600 in 2017 but the number for women has remained the same at around 700.
Recorded rates of infection did not differ significantly according to whether the surgery was an acute (unplanned) or elective (planned) procedure. However, rates of infection following acute surgery tended to increase with age whereas they tended to decrease with age for elective surgery. This may be explained by the small numbers of infections following major acute surgery for people aged 18–24.
Postoperative sepsis rates by DHB of service
- Postoperative sepsis is a serious complication of surgery and includes infections such as pneumonia or urinary tract infection that are not specific to the wound incision but do relate to the hospital stay.
- On average, there were 109.9 cases for every 10,000 major surgeries. This is a decrease from 119.8 in 2011.
- There was limited regional variation, although one DHB had consistently higher rates than the national average. Is this likely to reflect variable coding or genuinely higher infection rates?
- Women had significantly lower rates than men and rates tended to increase with age.
- There was no significant overall ethnicity difference in rates. However, Māori had significantly higher rates than non-Māori for women and 45–64-year-olds.
Rate of antibiotic dispensing within 30 days of major surgery in a public hospital by DHB of service
- On average, 32 percent of people were dispensed an antibiotic within 30 days of discharge after major surgery in a public hospital. This compares with an average of 2.3 percent of people being recorded as having an infection after major surgery in hospital.
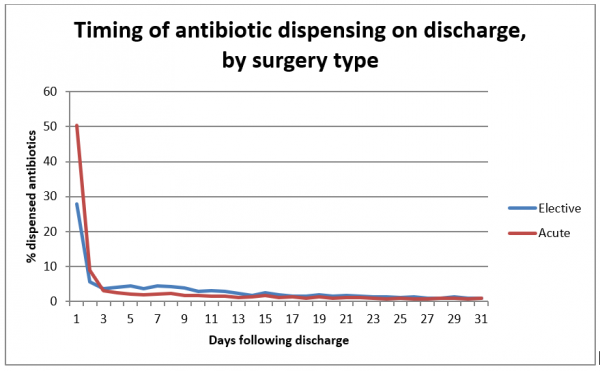
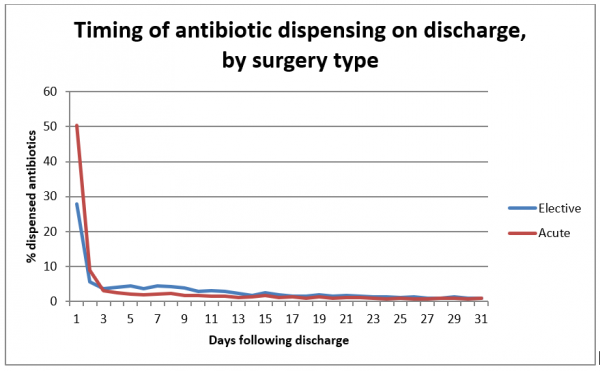
- As might be expected, antibiotic dispensing rates were significantly higher on discharge for people who underwent acute versus elective surgery – 37 percent compared to 28 percent. Since 2011, dispensing following elective surgery has decreased 6 percent, but still varies 2.8-fold between DHBs from 11.6 to 32 percent.
- There was a 2.2-fold variation between DHBs in the rate of antibiotic dispensing, from 18 percent to 39 percent of patients in the 30 days post-discharge.
- Rates of dispensing were significantly higher for men and for Māori. Rates of dispensing decreased with age.
- This pattern repeats for rates of dispensing following acute surgery but not for elective surgery. There were no significant demographic differences in rates for elective surgery.
- Almost half of the dispensing occurred on the same or next day of discharge after surgery. This raises questions such as how many scripts were for prolonged surgical antimicrobial prophylaxis or for treatment of superficial wound infections arising after surgery? How many scripts were generated in a follow-up appointment and what proportion was unrelated to the surgery but occurred because of hospitalisation?
People dispensed an antibiotic in the community in a month (2013)
- This indicator compares the rate of antibiotic use in the general community with those who may have an infection after health care treatment. Data were taken for a year with the monthly average presented. People were counted only once in a month in this measure, however one person may be counted in more than one month over a year.
- On average, 5.5 percent of people were dispensed antibiotics each month. This ranged from 4.5 percent to 6.8 percent of people. In 2011, 6.1 percent of people were dispensed antibiotics each month.
- Māori and non-Māori had similar rates in the age bands used in this Atlas. Antibiotic use was higher for Māori aged 45–64 than non-Māori but was lower for Māori aged 18–24.
- Those aged 65 and over received the most antibiotics.
- Māori women received significantly more antibiotics than non-Māori women but Māori men received significantly fewer than non-Māori men.
- When people dispensed antibiotics were counted only once in a year, 40.2 percent of people in 2017 aged 18+ had antibiotics dispensed one or more times.
What questions might these data prompt?
- Which types of surgery are most likely to result in an infection?
- Why is the rate of antibiotic dispensing after surgery high?
- Why are antibiotics being dispensed – is it for infection or prolonged prophylaxis?
Data for this Atlas domain were drawn from the Ministry of Health’s national hospital inpatient data (National Minimum Dataset, or NMDS) and Pharmaceutical Collection.
Infections after major surgery are a broader group than infections captured in the Commission’s Surgical Site Infection Improvement Programme, which applies the National Healthcare Safety Network definition (CDC 2015[2]). This requires active surveillance for infection and is a more robust method for identifying infections than using those reported in the NMDS. Identifying infections that occur in hospital relies on accurate reporting of these events and it is possible that some variation in rates may be the result of differences in recording. Infections that occur in the community post-discharge are not included unless they were severe enough to result in readmission.
The impact of length of stay is partially mitigated by only including surgeries that required a length of stay of at least two days, ‘major surgery’. This excluded minor or short stay surgeries such as elective hernia or carpel tunnel operations. In addition, people with a primary diagnosis of infection or sepsis were excluded; see the methodology (406KB, PDF) for a complete list of exclusions.
Infections included were: intra-abdominal infection, post-procedural infection, sepsis, stitch abscess, subphrenic abscess and wound abscess. The Pharmaceutical Collection contains claim and payment information from community pharmacists for subsidised dispensing. This collection does not allow for analysis of the patients’ condition or the effectiveness of dose provided, so it was not possible to assess the appropriateness or otherwise of prescribing; nor does it indicate if people took the dispensed medicine.
- Health Quality & Safety Commission surgical site infection improvement programme resources.
- Kazaure HS, Roman SA and JA Sosa. Association of postdischarge complications with reoperation and mortality in general surgery. Arch Surg. 2012 Nov;147(11):1000-7.
- Merkow RP, Ju MH, Chung JW et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015 Feb 3;313(5):483-95.
- NICE. nd. Surgical site infection – prevention and treatment. London: NICE. URL: http://pathways.nice.org.uk/pathways/prevention-and-control-of-healthcare-associated-infections#path=view%3A/pathways/prevention-and-control-of-healthcare-associated-infections/surgical-site-infection-prevention-and-treatment.xml&content=view-node%3Anodes-postoperative-phase (accessed June 2015).
- Norris P, Horsburgh S, Keown S et al. Too much and too little? Prevalence and extent of antibiotic use in a New Zealand region. J Antimicrob Chemother. 2011 Aug;66(8):1921-6.
- Thomas MG, Smith AJ and M Tilyard. Rising antimicrobial resistance: a strong reason to reduce excessive antimicrobial consumption in New Zealand. NZ Med J. 2014 May 23;127(1394):72-84.
- World Health Organization. 2011. Report on the Burden of Endemic Health Care-associated Infection Worldwide. Geneva: World Health Organization. URL: https://www.who.int/publications/i/item/report-on-the-burden-of-endemic-health-care-associated-infection-worldwide (accessed October 2018).
- CDC, Surgical site infection definition. URL: www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf (accessed October 2018).
- OECD. 2013. Health at a Glance 2013: OECD Indicators. OECD Publishing. doi: http://dx.doi.org/10.1787/health_glance-2013-en.
Introduction
Infection and antibiotic use following major surgery gives clinicians, patients and health care providers an overview of the following by district health board (DHB):
- infections after major surgery in a public hospital
- postoperative sepsis rates
- community use of antibiotics in the 30 days after surgery in a public hospital.
This domain was created to explore areas of wide variation between DHBs and identify possible areas for local quality improvement.
Healthcare associated infections (HAIs) are some of the most common adverse events in health care worldwide. Up to 10 percent of patients admitted to hospitals in the developed world acquire one or more infections.[1] HAIs include central line-associated bloodstream infections, catheter-associated urinary tract infections, surgical site infections and ventilator-associated pneumonia.
Summary
- Adherence to best infection prevention and control measures, such as choice of skin antisepsis agent, surgical antimicrobial prophylaxis and appropriate hair removal, are crucial to minimise the risk of surgical site infections.[2]
- Surgical antimicrobial prophylaxis should be administered for the shortest effective period to minimise adverse effects, the development of antimicrobial resistance and costs. In most situations, a single dose given 0–60 minutes before the surgical incision is all that is required. For some procedures, additional doses given for a maximum of 24 hours postoperatively may occur.
- It is not best practice for antibiotics to be administered routinely postoperatively – the UK National Institute for Health and Care Excellence (NICE) recommends antibiotics are used only in cases where infection is suspected.[3]
- The data suggest that, on average, 32 percent of people had antibiotics within 30 days of major surgery. This compares with an inpatient recorded rate of infection of 2.3 percent and postoperative sepsis of 1.1 percent.
- For people undergoing surgery, ask how to care for your wound after surgery, what signs of infection to look for, and when to seek help. If taking antibiotics ensure you know when and how to long to take them for. For more information click here.
Many HAIs can be prevented by adherence to best practice with well-established processes that minimise infection risk. However, not all HAIs are preventable or relate to the quality of care.
Other known risk factors for HAIs among hospital patients include prolonged hospital stay, prolonged and/or inappropriate use of antibiotics, immunosuppression and other severe underlying conditions.
This domain aligns with the work of the Accident Compensation Corporation and the Health Quality & Safety Commission’s infection prevention and control programme, which has a range of initiatives to reduce HAIs. These include improving hand hygiene, improvement related to peripheral lines, preventing central line-associated bacteraemia and reducing surgical site infections. All DHBs are involved in these initiatives.
Key findings
Note: This domain reports the number of infection events, not the number of people, thus one person may be counted multiple times. For all indicators (apart from indicator 8), patients were assigned to the DHB that provided treatment (DHB of service), not the DHB where they live. The risk of infection varies depending on the type of surgery and complexity of the surgical procedure. This means that DHBs with hospitals providing tertiary and quaternary services might be expected to have higher rates of infection, reflecting the higher complexity of surgical procedures performed. As an example, cardiac surgery is only performed in five DHBs.
Rate of infection following major surgery in a public hospital by DHB of service
- Infection is the most common complication of surgery; this indicator looks at infection rates directly linked to the surgery.
- In 2017, there was an average of 231 infections per 10,000 surgical discharges. This has decreased from 276 in 2011.
- Infection rates appear highest in the 45–64 age band. Rates have decreased in every age band from 2011 to 2017 except for the 25–44 band.
- There was no significant difference in infection rate between women and men.
- Māori had significantly higher rates than non-Māori, especially for women and 45–64-year-olds.
- There was limited DHB variation.
The total number of infections for men has reduced from around 700 in 2011 to around 600 in 2017 but the number for women has remained the same at around 700.
Recorded rates of infection did not differ significantly according to whether the surgery was an acute (unplanned) or elective (planned) procedure. However, rates of infection following acute surgery tended to increase with age whereas they tended to decrease with age for elective surgery. This may be explained by the small numbers of infections following major acute surgery for people aged 18–24.
Postoperative sepsis rates by DHB of service
- Postoperative sepsis is a serious complication of surgery and includes infections such as pneumonia or urinary tract infection that are not specific to the wound incision but do relate to the hospital stay.
- On average, there were 109.9 cases for every 10,000 major surgeries. This is a decrease from 119.8 in 2011.
- There was limited regional variation, although one DHB had consistently higher rates than the national average. Is this likely to reflect variable coding or genuinely higher infection rates?
- Women had significantly lower rates than men and rates tended to increase with age.
- There was no significant overall ethnicity difference in rates. However, Māori had significantly higher rates than non-Māori for women and 45–64-year-olds.
Rate of antibiotic dispensing within 30 days of major surgery in a public hospital by DHB of service
- On average, 32 percent of people were dispensed an antibiotic within 30 days of discharge after major surgery in a public hospital. This compares with an average of 2.3 percent of people being recorded as having an infection after major surgery in hospital.
- As might be expected, antibiotic dispensing rates were significantly higher on discharge for people who underwent acute versus elective surgery – 37 percent compared to 28 percent. Since 2011, dispensing following elective surgery has decreased 6 percent, but still varies 2.8-fold between DHBs from 11.6 to 32 percent.
- There was a 2.2-fold variation between DHBs in the rate of antibiotic dispensing, from 18 percent to 39 percent of patients in the 30 days post-discharge.
- Rates of dispensing were significantly higher for men and for Māori. Rates of dispensing decreased with age.
- This pattern repeats for rates of dispensing following acute surgery but not for elective surgery. There were no significant demographic differences in rates for elective surgery.
- Almost half of the dispensing occurred on the same or next day of discharge after surgery. This raises questions such as how many scripts were for prolonged surgical antimicrobial prophylaxis or for treatment of superficial wound infections arising after surgery? How many scripts were generated in a follow-up appointment and what proportion was unrelated to the surgery but occurred because of hospitalisation?
People dispensed an antibiotic in the community in a month (2013)
- This indicator compares the rate of antibiotic use in the general community with those who may have an infection after health care treatment. Data were taken for a year with the monthly average presented. People were counted only once in a month in this measure, however one person may be counted in more than one month over a year.
- On average, 5.5 percent of people were dispensed antibiotics each month. This ranged from 4.5 percent to 6.8 percent of people. In 2011, 6.1 percent of people were dispensed antibiotics each month.
- Māori and non-Māori had similar rates in the age bands used in this Atlas. Antibiotic use was higher for Māori aged 45–64 than non-Māori but was lower for Māori aged 18–24.
- Those aged 65 and over received the most antibiotics.
- Māori women received significantly more antibiotics than non-Māori women but Māori men received significantly fewer than non-Māori men.
- When people dispensed antibiotics were counted only once in a year, 40.2 percent of people in 2017 aged 18+ had antibiotics dispensed one or more times.
What questions might these data prompt?
- Which types of surgery are most likely to result in an infection?
- Why is the rate of antibiotic dispensing after surgery high?
- Why are antibiotics being dispensed – is it for infection or prolonged prophylaxis?
Data sources, method and limitations
Data for this Atlas domain were drawn from the Ministry of Health’s national hospital inpatient data (National Minimum Dataset, or NMDS) and Pharmaceutical Collection.
Infections after major surgery are a broader group than infections captured in the Commission’s Surgical Site Infection Improvement Programme, which applies the National Healthcare Safety Network definition (CDC 2015[2]). This requires active surveillance for infection and is a more robust method for identifying infections than using those reported in the NMDS. Identifying infections that occur in hospital relies on accurate reporting of these events and it is possible that some variation in rates may be the result of differences in recording. Infections that occur in the community post-discharge are not included unless they were severe enough to result in readmission.
The impact of length of stay is partially mitigated by only including surgeries that required a length of stay of at least two days, ‘major surgery’. This excluded minor or short stay surgeries such as elective hernia or carpel tunnel operations. In addition, people with a primary diagnosis of infection or sepsis were excluded; see the methodology (406KB, PDF) for a complete list of exclusions.
Infections included were: intra-abdominal infection, post-procedural infection, sepsis, stitch abscess, subphrenic abscess and wound abscess. The Pharmaceutical Collection contains claim and payment information from community pharmacists for subsidised dispensing. This collection does not allow for analysis of the patients’ condition or the effectiveness of dose provided, so it was not possible to assess the appropriateness or otherwise of prescribing; nor does it indicate if people took the dispensed medicine.
Recommended reading
- Health Quality & Safety Commission surgical site infection improvement programme resources.
- Kazaure HS, Roman SA and JA Sosa. Association of postdischarge complications with reoperation and mortality in general surgery. Arch Surg. 2012 Nov;147(11):1000-7.
- Merkow RP, Ju MH, Chung JW et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015 Feb 3;313(5):483-95.
- NICE. nd. Surgical site infection – prevention and treatment. London: NICE. URL: http://pathways.nice.org.uk/pathways/prevention-and-control-of-healthcare-associated-infections#path=view%3A/pathways/prevention-and-control-of-healthcare-associated-infections/surgical-site-infection-prevention-and-treatment.xml&content=view-node%3Anodes-postoperative-phase (accessed June 2015).
- Norris P, Horsburgh S, Keown S et al. Too much and too little? Prevalence and extent of antibiotic use in a New Zealand region. J Antimicrob Chemother. 2011 Aug;66(8):1921-6.
- Thomas MG, Smith AJ and M Tilyard. Rising antimicrobial resistance: a strong reason to reduce excessive antimicrobial consumption in New Zealand. NZ Med J. 2014 May 23;127(1394):72-84.
References
- World Health Organization. 2011. Report on the Burden of Endemic Health Care-associated Infection Worldwide. Geneva: World Health Organization. URL: https://www.who.int/publications/i/item/report-on-the-burden-of-endemic-health-care-associated-infection-worldwide (accessed October 2018).
- CDC, Surgical site infection definition. URL: www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf (accessed October 2018).
- OECD. 2013. Health at a Glance 2013: OECD Indicators. OECD Publishing. doi: http://dx.doi.org/10.1787/health_glance-2013-en.
